Pizza as a Vegetable and Other Roadblocks to Proper Nutrition

Photo by Ben+Sam.
In Brooklyn’s PS 321 in Park Slope, it is second-grade lunch period and the adjoining lunchrooms are a controlled cacophony of happily eating kids. Children carefully balance trays from the cafeteria to the long white lunch tables. On those trays a small apple wobbles beside a grilled cheese sandwich, a serving of salad and some mixed cooked vegetables.
The cafeteria has a water cooler and twin water fountains, as well as crate full of small cardboard cartons of milk. On one wall display the word “Yum” hangs below photos of smiling students eating fruits and vegetables. The school, which serves over 1,400 kids in pre-K through 5th grade, incorporates a “healthy choices month” into their classroom learning. They also uses students to talk to other students about what is and isn’t good in their lunches, and works with school food staff to incorporate those findings into meal planning.
Despite the success of efforts like those at 321, school officials and health advocates still face many obstacles to getting children to eat better. Even the best school lunch program can falter in the face of all the junk food options available on city streets and in the disdain of notoriously picky eaters. And, as the recent vote by Congress to consider pizza a vegetable makes clear, institutional obstacles remain as well.
Assistant Principal Ryan Bourke says PS321 works to teach students the importance of healthy eating. In an organic garden in the school yard, kids learn about growing vegetables, and occasionally parents come harvest those crops into salads for students to sample. While the majority of students bring their food from home, Bourke says he believes that to be changing, especially when certain foods are offered. “Pizza day they love,” he said, smiling. “Chicken they love.”
In October, Manhattan’s P.S. 75 on the Upper West Side became the first school in New York City to receive a HealthierUS School Award. The school added more fruits, vegetables and whole grains to kids’ lunch, and also installed a water cooler, earning them a bronze award. The school’s website offers “snack guidelines” for parents, to guide them in the sorts of foods they send their child to school with. The guidelines encourage parents to send kids to school with a refillable water bottle, and discourage things like store-bought muffins and fruit roll ups.
While not all schools have the resources to provide students with these sorts of experiences, citywide regulations on school food are among the strictest in the country. Regulations like the 2009 ban on most bake sales also place limits on what can be sold in school vending machines and stores.
An Uphill Battle
Yet even the healthiest of school options cannot negate the options available after school. A recent study from researchers at Columbia University’s Mailman School of Public Health looked at the availability of junk food sold near public schools in the city, using data on school locations from 2006-2007. The abstract gives a lot of insight into why healthy school lunches are only one step toward maintaining healthy children.
The researchers found that 92.9% of students had a small grocery store within 400 meters of their school; these stores typically carry fewer healthy food options than larger grocery stores. In addition, 70.6% had a pizzeria within 400 meters, 48.9 % were that close to a convenience store, 43.2% were within 400 m. of a national chain fast-food restaurant, such as McDonald’s or Burger King, and 33.9% were within 400 m. of a local fast-food chain restaurant.
Even in affluent Park Slope, where students who go off campus are more likely to purchase healthy foods like sushi than a McDonalds hamburger, schools hope to encourage more eating of school food. PS 321 has recently been engaging in an effort to destigmatize school lunches and eating in the cafeteria. They are working to find healthy foods that kids like, and limiting the number of days that older students are allowed to eat lunch off campus.
Offering food that kids like is a big part of steering students away from the fast-food. While some schools seem to do that quite well, others have been less successful. At the Young Women’s Leadership School in Astoria, students have created a blog about the quality of the food, and while many of their comments seem to express normal kid pickiness, a look through the posted photos is instructive.
Removing sodas from school may not have the hoped-for effects on children’s health either. In a nationwide study published in The Archives of Pediatrics and Adolescent Medicine, researchers found that in schools which banned soda but allowed other sugary drinks, students just consumed more sugary drinks. More alarmingly, in states that banned all sugary drinks in schools, students’ overall consumption of sugary drinks still remained constant –the kids just upped their intake elsewhere.
Then there is the issue of pizza as a vegetable. This month Congress blocked an effort by the Agriculture Department to create stricter guidelines to ensure that schools served fruits and vegetables. Currently schools are able to claim credit for serving a vegetable even for the watered-down tomato paste present on a slice of pizza. The New York Times reports that food companies including ConAgra, Coca-Cola and frozen pizza-maker Schwan praised the decision as reasonable.
Here in New York, Amie Hamlin is not pleased by the decision. “The whole point” says Hamlin, frustration audible in her voice, “is to have more nutrient-rich vegetables that are low-calorie.” Blocking it, she says, was “really dumb.”
Hamlin is the Executive Director of The New York Coalition for Healthy School Food (NYCHSF),a statewide nonprofit that advocates for healthier plant-based school lunches and increased school nutrition education. In New York City, NYCHSF partners with others to bring whole-food healthy recipes into 17 NYC public schools, twice a week. Her organization provides recipes that use ingredients that schools already have access to, and trains staff in how to prepare them. They also provide a “Wellness Wakeup” program, giving principals short bits of nutritional information to be read over school intercoms in the mornings.
Not every school in New York City has a cafeteria, and not every cafeteria has cooking facilities. Hamlin estimates that in NYC’s 1500 schools there are about 1200 cafeterias, due to colocation of multiple schools in a single building. Of those, some are only equipped for reheating and serving.
Still, Hamlin says, the demand for healthy food in schools is strong. While her organization only serves 17 schools, there are 48 more on the waiting list. Hamlin says NYCHSF is constrained by a lack of funds and volunteers. “We need more people power to do it,” she says, adding that volunteers with NYCHSF also go into school lunchrooms with the raw ingredients of the meal, to allow students to touch and see and smell the foods. The organization plans to collect data regarding how much of their food is consumed or thrown away.
Income-eligible in New York City public schools are entitled to eat lunch for free or at a reduced rate of twenty-five cents, other students pay $1.50. That price may increase next year due to a provision in the federal Child Nutrition Bill that mandates that the price of school lunches better reflect the cost of preparing the meals. Those higher prices may pose a challenge for families ineligible for the reduced rate but still struggling financially. DOE spokeswoman Marge Feinberg said it is “too soon to know” whether New York City students will have to pay more next year, but pointed out that it costs the Department $2.60 on average to produce a meal.
DOE would not permit an interview with the Steven O'Brian, the Director of Food and Food Support, but sent a statement saying New York Schools are “ahead of the curve when it comes to making school food more nutritious” and citing their efforts to eliminate trans fats and reduce sodium, fat and calories. “The Department serves over 820,000 meals a day and purchase a large volume of goods each year. For example, we purchase 15 million apples a year, 400,000 pounds of chopped Romaine lettuce and 4,000 pounds of cucumbers, 99,000 pounds of broccoli florets, to name a few. “
Still, the Department has no way to track what gets eaten and what gets thrown away. The reticence of the Department to speak to the press may be due to recent criticisms brought on after a school food internal website with nutritional value for the food was accidentally made public. The site was quickly removed and the link now brings up a message that the file or directory is not found, leading some critics to wonder why the DOE would not release nutritional information to parents.
Back at PS321, kids are finishing lunch and squirming onto their jackets in anticipation of the playground. Patient lunch aides help locate hats and zip zippers. Several second graders hop up and don badges designating them as Healthy Kids Café Student Representatives. One representative, a tall pretty girl with bright plastic beads in her braids, circles the room, seeking out the kids with school lunches and asking them how they liked the food. One after another after another, the students give her a thumbs-up and a smile.
30 Years of Fighting AIDS: Much Progress, Many Losses

Photo by Eddie O.
Part one of two. For part two, go here.
In 1984, when Jim lost his 22-year old boyfriend to AIDS, he didn't think he would live to see 30. When he was diagnosed with HIV himself five years later, Jim never expected to turn 40. He had stopped counting how many friends had died when that number reached 200.
The medication available at the time, AZT, was supposed to be taken three times daily, but Jim could not handle even a portion of that dose without getting sick. So he put off treatment until 1997. By then Jim's T cell count was below 200, the demarcation for HIV turning into AIDS. Fortunately, antiretroviral medications -- much more powerful drugs with fewer side effects -- were just being approved, and Jim's reaction to them was quite good. His T cell count soon rose to 350.
Today, 21 years after being diagnosed with HIV, Jim, at 57, is still with us, and his outlook for the future is much improved.
Jim is not alone. Like Jim, Keith (not his real name), who was diagnosed with HIV in 1994 at age 29, also never thought he’d still be here.
"There's a lot of us," Keith said. "I think something else will kill me before HIV. I know people who are still alive who have had the illness now for 20 to 25 years and longer, from the 1980s. … It's not on my radar to die from HIV any longer."
More than 30 years after the first known death from AIDS in New York City – and on the eve of World AIDS Day – much has changed since the epidemic ripped through the city in the 1980s. Major advances have been made in treating HIV and AIDS, and social service agencies have stepped in to meet the needs of many HIV positive people who need help.
Yet challenges remain. Every year some 1,000 New Yorkers still are diagnosed with HIV so late it has already become AIDS. Many others go untested –- and undetected. And the city must now deal with a population many thought it would never have to serve: aging people with HIV/AIDS.
By 2015, over half of people in the United States living with HIV will be over the age of 50. In New York City, almost 40 percent of the estimated 107,000 New Yorkers living with an HIV/AIDS diagnosis are over age 50, and 75 percent over 40.
Their longevity is testimony to the success of what has been done to combat HIV/AIDS. Living with HIV into middle age and beyond, though, presents another set of issues: medical, financial, social and personal.
Knowing Helps
Youth, particularly young men having sex with men, are still seriously at risk for new infections. Even though, overall, new HIV diagnoses in the city have decreased, they continue to rise among the young, particularly young gay and bisexual men. And African American men, ages 13 to 29, experienced the greatest increase in new infections in 2009: 48 percent.
Knowing your HIV status and, if you are HIV-positive, getting access to the life-saving drugs are prerequisites for survival. With that in mind, the city and state have taken steps to tell people about the tests and increase their availability.
"Once people become aware of their HIV-positive status," Rod McCullom wrote for the Black Aids Institute, "not only are they more likely to take steps such as using condoms to avoid infecting their sexual partners, but research now shows that beginning treatment soon after diagnosis makes people with HIV/AIDS significantly less infectious."
Last year, New York state passed a law requiring that HIV testing be offered to people aged 13 to 64 in primary care, hospitals or emergency rooms. Patients can refuse the test. The city now mandates sex education classes in public schools for middle and high school students that will include curriculum about unprotected sex and how to use condoms.
And the city health department has come out with a graphic public service announcement, “It's Never Just HIV," illustrating the other medical problems that often accompany HIV in an attempt to curb complacency and urge viewers to use condoms.
Reducing Risks
Over the years, targeted programs have helped drive down new infections among at risk groups.
Intravenous drug use -- once a major means of transmission of HIV in the city -- has been reduced to 4.4 percent of new HIV diagnoses owing largely to syringe exchange programs that allow adults to purchase up to 10 needles without a prescription from a pharmacy or to obtain them from registered health care facilities. The state also recently changed its penal law so that possession of a residual amount of a controlled substance in or on a syringe is no longer a crime, although there are still reports of police harassment around needle exchange programs. Advocates would like to see more efforts to train police on the benefits of needle exchange.

Photo by angelsinamericacostumes
Doctors at Harlem Hospital in 1986 monitor an HIV positive baby's condition. Testing and treatment of infants has essentially eliminated HIV among babies in New York.
Mother-to-baby transmission has been virtually eliminated in New York state by mandatory testing of all babies born, if the pregnant mother has declined a test, followed by immediate treatment — which can expel the virus in two-thirds of the infants — when HIV is present.
But while the youngest New Yorkers get tested, older ones frequently do not. This is true even though people over 50 account for 17 percent of the new diagnoses of HIV in New York.
African Americans over 50 are 12 times as likely as their white peers to contract HIV, and Latinos are five times as likely, according to a Centers for Disease Control publication. African American women over the age of 50 make up 65 percent of all women with HIV and 67 percent of new diagnoses among women in New York City. Three quarters of these woman report unprotected heterosexual sex as the means of transmission.
In December 2009, the federal government announced that Medicare will now cover HIV screening tests for people over 65.
Every step forward, however, highlights the gaps left behind. For example, the Centers for Disease Control issued a recommendation that all people aged 13 to 64 year get annual HIV tests . “Great!” said Nathan Schaefer, director of public policy at the Gay Men's Health Crisis. But, he added, the government should recommend HIV tests for all ages, particularly in light of Medicare's decision to make HIV testing available to those over 65.
The lack of tests speaks partly to the common assumption that seniors do not have sex, even though a 1998 study by the National Council on Aging found that 61 percent of men and 37 percent of women over 60 were still sexually active. Those numbers probably have increased with the erectile–dysfunction pills now available.
Adults over 50 at risk for HIV were 80 percent less likely to be tested as at-risk adults 20 to 30 years of age, according to one study.
Doctors may not ask their older patients if they are sexually active. Men over 50 who are having sex with other men, afraid of anti-gay bias, may not disclose this to their doctor. Women who have entered menopause, no longer concerned about pregnancy, often will not use protection and will seldom discuss this with a health-care provider.
Older people's symptoms of HIV/AIDS were also frequently misdiagnosed as other illnesses. "Sometimes the effects of HIV among older adults, such as fatigue and cognition loss, are perceived to be just part of aging process," said Schaefer.
Because many older adults are not tested they may only discover they have HIV while being treated for other conditions. Frequently, this is long after they contracted the illness, so it has progressed to AIDS and likely been transmitted to others.
"The CDC really needs to develop a preventive program targeted for older adults," said Schaefer. "Current CDC models for prevention for high risk populations do not include seniors. These models … have been demonstrated to be efficacious and are used to shape new prevention programs. But not one has been designed for older adults."
After the Test
Testing enables people to get help sooner, increasing their chances of survival. But many need government assistance as well.
Ethan (not his real name) was diagnosed with HIV in 2005, at age 56. He is 62 now. "At first my T cell count was very high. I was still healthy from a statistical point of view. So I was able to distance myself. Yeah, I got it, but I don’t need medication. And that was a source of pride," he said.
He delayed going on the drugs, but, he continued, "Every time I had blood work done, my T cell count was going down. … I was very weak. I realized it finally became time to go on the medications."
When Ethan handed the prescription to the pharmacist, he was told that his insurance company was not going to pay for it. “The pharmacist told me I had $1,000 annual limit on medication. Just one of the medications the doctor was prescribing, to keep me from getting pneumonia, would cost $3,000 a month.
Fortunately, Ethan's doctor figured out that Ethan would qualify for AIDS Drug Assistance Programs or ADAP. As a result, Ethan said, "I finally got on the medications and I got stronger."
ADAP is one of the many programs established in the last 30 years to assist people with HIV/AIDS. New York, more than many other states, does try to provide some kind of a safety net to people with the virus.
"We're fortunate to live in a state that is so dedicated to good health care," said GMHC's Schaefer. With states across the country cutting their budgets, Schaefer said, "a lot of states are experiencing more need than they are able to meet" and have waiting lists for medications. These states, according to Schaefer, "are not able to put up the money to make the required dollar match to pull down the maximum amount of federal reserves. But New York does."
The help extends beyond medication. Once Keith began treatment, he never had a problem getting services and help in the city. After he was laid off from his job, he applied for public assistance through the HIV/AIDS Services Administration, or HASA, an organization that helps folks diagnosed with AIDS or symptomatic HIV find emergency housing, financial assistance, medical care and other services.
"New York state is really great," said Keith. "I thought for years about moving away, for various reasons, but because of the care here -- my doctor, the medications, the services -- I won't." He said he also has gotten " wonderful support" from three nonprofits: GMHC, Friends in Deed, a support organization for people affected by life-threatening illness; and the New York Buyers Club for nutritional supplements.
Still in Need
But not everyone in New York has thrived. HIV related illness is the number one cause of death for women in New York City’s shelter system, according to a 2005 reportfrom the city health department and the Department of Homeless Services.
"Affordable and stable housing is a serious priority for people living with HIV," said Schaefer. "Studies show that if someone is permanently housed, the outcome is better in every way. "
With housing costs so high in New York, finding that stable situation can pose a challenge.
The neighborhood you live in also may put you at risk. People living in neighborhoods with high rates of poverty, substance abuse and sexually transmitted disease. as well as a prevalence of HIV and low rates of testing, are at high risk for HIV infection. These neighborhoods include Central Brooklyn, Harlem, the South Bronx, Hell’s Kitchen, the West Village and Chelsea. All except Chelsea also have high death rates associated with AIDS. Lower income communities face higher death rates than other areas with similar HIV prevalence.
Part one of two. For part two on aging with HIV and budget challenges, go here.
Aging with HIV: A Triumph with Challenges
Part two of two. For part one on advances in treatment and the changing face of people with HIV and AIDS, go here.
Complicating the situation is the current recession. Funding cuts to programs that support people living with HIV are in the latest New York City budget, including a $1.3 million cut in the HIV/AIDS Services Administration's rent assistance program,. The city also cut HIV prevention and health literacy for seniors, HIV/AIDS Communities of Color and money for the Injection Drug Users Health Alliance.
The New York state budget has instituted a ceiling on payments to Certified Home Health Care Agencies that serve people with special needs, including those with HIV/AIDS. The budget also includes a cap on the Medicaid pharmacy benefit and a policy change that gives the state authority to deny coverage on certain drugs.
Just this month, the federal government reduced the Housing Opportunities for Persons With Aids program by $2 million and, as Congress has yet to pass a budget that would reauthorize funding for the AIDS Drug Assistance Programs.
Aging with AIDS
The cuts come as agencies confront the rise of HIV/AIDs among the elderly and soon to-be elderly.
Comorbidity -- other illnesses surfacing and existing simultaneously with HIV/AIDS -- is common for someone living with HIV, either as a result of the weakened immune system or as a side effect of the antiretroviral mediations. Heart disease, osteoporosis, diabetes and cognitive dysfunction are some of the conditions that can surface. Depression is twice as common among people living with HIV, particularly older adults, than with the general public, as is a higher incidence of substance abuse.
Nausea, diarrhea, fatigue, lipodystrophy (a redistribution of fat in the body), elevated cholesterol levels, neuropathy and kidney disease can all be side effects of the medication.
"Is it HIV or is it aging?" James Masten asks in his recently published book Aging with HIV: A Gay Man’s Guide. The answer is not always evident and may require research and reflection.
Masten also addresses the "triple threat" that gay men over 50 who are living with HIV have to face: homophobia, HIV/AIDS and ageism. There is stigma at every turn.
Aging means changing, said Masten, and adapting to those changes is key, along with self-care and reestablishing a network of friendship and community. Embrace life, he counsels, and keep it simple.
Schaefer highlighted a number of recent successes for folks aging with H.I.V., including City Council support for sensitivity training for health and human service providers, and for senior center leadership staff, to counteract stigma and discrimination . The city also awarded SAGE (Services and Advocacy for GLBT Elders) a contract to open the first lesbian and gay senior center in New York starting in January 2012.
HIV/AIDS at 30: Grieving and Moving Forward
"The fact that we are dealing with H.I.V. and aging issues is a huge advancement in itself," said Schaefer. “Twenty years ago we weren’t speaking of living with HIV in people 50, 60 and 70."
As Masten writes in his book, “The 1980s and 1990s were a holocaust for gay men."
The tragedy of those years still deeply affects those who lived through it.
Unacknowledged emotions -- such as grief, stigma, survivor's guilt and shame --are barriers to optimal aging with HIV," said Masten. "They prevent the adaptation of self-care strategies and aid in the creation of a shrinking life." Optimal aging, Masten suggests, involves rediscovering how you want to live your life.
For Jim, pleasure comes from being an activist. "I'm a late bloomer in terms of doing advocacy, putting in that effort, meeting with politicians," he said. "Even if every campaign is not a success, being able to expend my energy in that way instead of becoming depressed and escaping by diving into some type of addiction -- which will just kill you faster -- makes me feel like I have some control and that I'm contributing to what will be a positive outcome."
The day he was diagnosed with HV, Ethan had an insight that there would be love and support for him as he walked through this. Going forward into his future, he finds the issue is often, "Can I accept that love and support?"
Keith enjoys his 14-year-old poodle, his family and friends, and volunteering at a meditation center. And, he said, "not a day goes by where I don't have gratitude, for everything in my life, but especially just to still be alive. Every moment, whether great or difficult, I am just content to still be able to experience. It really can't get any better."
Top Hospitals Offer Separate and Unequal Care

Photo by Susan NYC
By almost any measure, people of color suffer worse health outcomes than their white counterparts. The contributing factors vary, ranging from lack of access to healthy food to taking fewer preventative health measures.
On Tuesday, the New York State Medicaid Redesign Team voted on a slate of proposals to reduce disparities in healthcare in the state. One of them attempts to tackle the thorny problem of separate and unequal access to health care for people on Medicaid at some of New York's most elite private hospitals -- a problem we call "segregated care."
In New York City, the type of specialty outpatient care a person receives is often dictated by how they pay for that care Private academic medical centers, also known as teaching hospitals, are partly to blame for this.
People who have private insurance go into one system. Those with no insurance or with public insurance such as Medicaid go into another. Because African-Americans and Hispanics in New York City are more than twice as likely as whites to be publicly insured or uninsured, patient steering by insurance status disproportionately hurts people of color. Whether intended or not, this two-tiered system amounts to racial discrimination.
New York State Sen. Gustavo Rivera and Assemblymember Nelson Castro, both of the Bronx, have introduced legislation that gives New York the chance to right this wrong and make health equality a reality. The proposal voted on by the redesign team is based on this legislation. Together, these measures could substantially improve access to health care for millions of New Yorkers.
The Second Tier
In New York City, private academic medical centers, which unlike community or public hospitals also run their own medical schools, operate a two-tiered system. Privately insured patients are seen in faculty practices, while those on Medicaid or uninsured are seen in outpatient clinics. (Because public hospitals largely cater to Medicaid or uninsured patients, segregated care is a non-existent issue in these institutions.)
Worse still, the academic medical centers do not ensure that Medicaid patients seen in the clinic have access to the same services or quality of care as privately insured patients. In the clinic system, patients are usually treated by residents on a rotating schedule. This makes continuity of care, which is linked to reduced hospitalization and earlier identification of chronic disease, difficult. Other issues, such as long waiting times for appointments, limited coordination between specialists and primary care doctors, and lack of night or weekend coverage, continue to plague the clinic system and the patients who shuffle through it.
To document this segregation, Bronx Health REACH conducted two telephone surveys of several major hospitals in New York City. The callers phoned four different specialty departments (cardiology, endocrinology, ophthalmology, and nephrology) to try to make an appointment for a relative. In almost every instance, the first question the caller was asked was what insurance their relative had. If the answer was private insurance, the caller was always referred to a private practice. Callers who stated their relative had Medicaid or no insurance were almost always referred to the clinic system.
Bronx Health REACH and New York Lawyers for the Public Interest have been fighting to end segregated care for over a decade. Other avenues, including a civil rights complaint filed in 2008 with the New York state attorney general, have not proved successful.
The introduction of the legislation in June by Rivera and Castro in both houses of the legislature is a major step forward. The statewide bill would prohibit steering of patients into different care settings based on insurance type and instead require that patients be treated by integrated care teams. It would also mandate that hospitals inform patients of financial assistance programs and require that academic medical centers negotiate with Medicaid managed care plans so that all providers are eligible to treat Medicaid patients.
"In New York state, we have the opportunity to go a step further than the national health care legislation requires by addressing health inequities that exist based on an individual's ability to purchase quality healthcare insurance," Rivera said. He said the bill, which Bronx Health REACH helped initiate, "will further chip away at policies that create health disparities along class lines, and will work toward ensuring that quality healthcare be a basic right for all New Yorkers."
Separate and Not Equal
Though our phone surveys determined that private hospitals do separate patients based on insurance status, hospitals have argued that separate doesn't necessarily mean unequal. In meetings with hospital administrators over the years, Bronx Health REACH and attorneys from New York Lawyers for the Public Interest have received a number of vague responses about why the two-tiered system continues to persist.
Administrators have said that this is how it has always been done. Some administrators, and even some doctors, have implied that the clinic patients should be grateful for what care they do get.
Hospitals also have cited financial considerations, arguing that Medicaid does not reimburse enough for visits to private doctors' offices. This may be true, but it's not the whole truth. Medicaid reimburses at a higher rate for a patient seen in a clinic than at a private doctor’s office. If a faculty or attending physician saw patients in a clinic setting, they would receive the higher rate and the patient would get the high quality care afforded to privately insured patients.
The Effect on Patients
Bronx Health REACH's work in underserved communities throughout New York City has uncovered countless stories of unequal treatment in outpatient clinics.
Vanessa Ghigliotty was a 27-year-old single mother from the Bronx when she went to the doctor in May 2001 to find out why she was always tired. As a Medicaid beneficiary, she went to her usual place of care, a hospital clinic. The doctor told her that she had been working too hard and advised her to take it easy for the summer.
The summer passed, and Ghigliotty still felt incredibly fatigued. Meanwhile, a growth that hurt to touch had formed on the right side of her stomach. In October, she went back to the same clinic and saw a different doctor, who rather than running any tests, told her she needed to eat more roughage and lose weight. He attributed the bulge to gas, even though Ghigliotty told him she was concerned because it was rock hard and very tender. The doctor dismissed her concerns and suggested she pick up a new hobby and find a boyfriend.
By April 2002, Ghigliotty could no longer walk. Though in constant pain, she was terrified to go back to the clinic and receive the same dismissive treatment. Her parents finally convinced her to go to the emergency room, where she learned she had Stage 4 colon cancer. Eventually, Ghigliotty got treatment for her advanced cancer at Memorial Sloan-Kettering and underwent four and a half years of chemotherapy and seven surgeries.
"When I first went to the doctor, I probably had Stage 2 cancer, but then I had to wait almost a year and it was everywhere," she said. "I think that's what the problem is in clinics. You get largely ignored until you can't ignore it anymore, until it's impossible to ignore."
For Gary Spears, a pastor from the Bronx, a small cut on his finger turned into a massive infection. Concerned, Spears went to the emergency room, which referred him to the hospital's outpatient clinic. They sent him home with some Tylenol and a bandage. The infection continued to get worse, and Spears kept returning to the clinic, where he saw a different doctor each visit.
At the time, the reverend had experienced rapid weight loss and was constantly tired, had trouble eating and needed to go to the bathroom frequently. Despite these all being signs of diabetes, especially in people who are overweight, the medical staff never gave Spears a blood test to determine if his glucose levels were too high.
Luckily, at his church Spears met a doctor, who noticed his bandaged hand and made him an appointment for the next day. Spears got a finger stick and found out he was a diabetic and at risk for amputation. Through proper intervention and treatment, Spears was able to keep his finger and get his diabetes under control.
"Every time I went for a follow-up, or to let them know how I was doing, I saw a different doctor. And that doctor appeared not to be looking at the charts until he got into the room," said Spears. "I felt I wasn’t being cared for, and I was wasting my time. I was waiting for long periods of time to be seen, and then I was not getting treated like an individual."
One System for All Patients
Integrated specialty care systems are not a radical pipe dream. At academic medical centers in other areas of the country, including at Massachusetts General Hospital in Boston, the same doctors see all patients, regardless of insurance, in the same place. This integrated approach is not only equitable, but it does away with a wasteful system where hospitals operate two specialty-care practices under the same roof.
In addition, under the Hill-Burton act and other laws, academic medical centers, which receive millions of dollars in federal and state funding, must make their services available without discrimination, especially to recipients of Medicaid. Instead, by providing a separate system of care with poor access to specialty services, these hospitals are practicing blatant discrimination against a population that is largely low-income and racially and ethnically diverse. The failure of academic medical centers to participate in many of the Medicaid managed care plans available in New York, despite the fact that 90 percent of Medicaid recipients in the state are mandated to participate in managed care, further discriminates against this underserved population.
The medical community does have guidelines that address these concerns explicitly. The New York State Patients’ Bill of Rights states that patients have a right to "receive treatment without discrimination as to race, color, religion, sex, national origin, disability, sexual orientation, source of payment, or age." (Italics added.)
The New York State Department of Health has also issued guidelines for medical residents as specialty-care providers for Medicaid managed care patients. These guidelines require that patients be given the name of the attending physician in writing, even if they are seen by a resident. All patients have a right to be cared for directly by the attending physician if they request it. The guidelines also require that Medicaid enrollees in specialty outpatient clinics be cared for in a setting that allows for continuity of care and have the ability to make follow-up appointments with a particular resident or attending physician. In addition, the guidelines state that training sites must integrate the care of Medicaid, uninsured and private patients in the same settings. While these guidelines are in place, they are not enforceable nor have they been followed.
The Health Equity Bill now in the legislature, and the Medicaid Redesign Team proposal going before Gov. Andrew Cuomo for possible inclusion in his budget, would eliminate the separate and unequal system of care in favor of an integrated system that delivers the highest quality of care to all patients, not just those with private insurance. Without it, the New York City private teaching hospital system, considered by many to be one of the best in the world, will continue to cater to the white and affluent, leaving the publicly insured and uninsured to manage high need chronic conditions without quality medical care. We can do better.
Charmaine Ruddock is project director of Bronx Health REACH, community coalition funded by the Centers for Disease Control and Prevention and dedicated to the elimination of racial and ethnic health disparities.
Is the City Prepared to Help Returning Veterans?

Photo by Alec Hamilton
At age 17, Selena Coppa enlisted in the military through the Delayed Entry Program, a program that allows people too young to enlist to promise to enter the military once they are of age. The Brooklyn native says she joined out of a strong sense of service to her community. “I wanted to give something back in exchange.” she explains.
She served for eight years in the United States Army, working as an intelligence analyst, a platoon sergeant, and an intelligence squad leader, before returning to New York City two years ago.
Shortly after she returned, Coppa began experiencing symptoms of post-traumatic stress. She began having nightmares, and would startle awake at any sound. She would hear or see something, and suddenly be immersed in forceful memories of combat. More and more often she would find herself needing to quickly leave a situation in order to calm herself down, and that began taking a toll on her work and her school.
A single mother, Coppa has struggled to find adequate healthcare for herself and her young daughter. Yet despite being aware of the services offered through the VA hospital and the city, Coppa says she avoids using them. The crowds often present at city clinics trigger her PTSD, and she has concerns about the quality of care in both city clinics and the VA. In desperation she brought her daughter to a city health clinic to get sutures once, but was so unhappy with the situation that she spent more than she could afford to take her child to a private doctor for the follow-up.
Last year Coppa fell sick with a particularly violent flu. After waiting several hours to be seen at the VA, Coppa gave up and tried to return home. On her way home she passed out on the sidewalk in Brooklyn, and dropped her purse. Strangers helped her home and no one stole her bag.
One in Eight
The greater New York City area is home to an estimated 1.3 million veterans. The highest numbers of veterans are currently in Queens, with an estimated 225,370 veterans, followed by Brooklyn, Manhattan, and then the Bronx and Staten Island.
This number is about to increase sharply as thousands of veterans return from service in Iraq and Afghanistan. A demographic analysis of recruits by the Heritage Center found that the Bronx and Brooklyn were among the ninety-nine ZCTA (zip code tabulation areas) to have sent the most recruits into the military in 2003. In addition, as of 2009, there were 26,240 people on active duty in New York State and 39.353 or reserve and National Guard.
As operations Iraqi Freedom (OIF) and Enduring Freedom (OEF) wind down, the city will experience a surge in younger veterans. Many of these will struggle with unprecedented levels of psychological health problems as a result of extended deployment and severe violence. Yet at the same time those veterans are returning home, to a bad economy and a city that is facing budget shortfalls resulting in reduced services.
The Mayor’s Office of Veteran’s Affairs seems ill prepared to deal with the influx of new troops and their needs. MOVA currently operates on a $500,000 annual budget, $400,000 of which goes to employee salary, according to the testimony of Commissioner Terrance Holliday. And the commissioner has been unable to explain what help his office has provided to returning troops that need mental health services.
Asked by City Councilmember Dan Halloran to name what MOVA has done to address issues of mental health services, Holliday was only able to say that his department had organized an outreach event, but could site no other effort. He did say that the agency was spending a lot of “energy and personal capital” on getting people into jobs. In addition he testified that to his knowledge the veterans his organization served had all had positive interactions with the VA, though he was unable to quantify even roughly, how many veterans his agency had helped.
Yet Commissioner Holliday testified that MOVA hasn’t had a problem with lack of funding. Councilmember Halloran was astounded by that response. “The city spent four times that amount on the condom campaign.” he said. “As a veteran, you don’t have a problem with that?”
The commissioner shook his head. “As a veteran, I do not.”
Hard times in the city have made for hard times for the local agencies and nonprofits that provide services for the city’s vulnerable. Suicide prevention service The Samaritans of New York saw their twenty-year contract with the DOHMH cut completely, only to be restored by the City Council. Executive Director Alan Ross said of the cuts “We went from helping people in crisis, to being in crisis.” While Samaritans does not provide services geared specifically for veterans, their plight is indicative of that of many nonprofits in the city.
Unique Needs
Returning veterans can face a wide variety of mental and physical health challenges, and may have unique needs resulting from their service. Those physically injured during their time in the military may have challenges regarding self-care or transportation, requiring service ranging from minimal to intensive. At the same time, many veterans are returning with the less visible wounds of mental trauma, wounds which can be devastating for the individual as well as their families and communities.
Recent studies have indicated a high prevalence of mental health issues in returned service personnel. A recent memo from the Samaritans of New York suicide prevention organization claims that more American soldiers are dying from suicide than from warfare. The memo quotes a Rand Corporation study that found that nearly 20 percent of US service members returning from war will report symptoms of PTSD or major depression, but only 53 percent of those will seek help. The study sites both gaps in services and stigma around seeking help as factors.
Coppa’s experience backs up those findings. Many veterans with PTSD have trouble dealing with bureaucracy and complicated paperwork, and as a result are disqualified from services for which they should be entitled. Coppa said veterans who try to access city services may also encounter a barrier in the requirement by some services of proof of residency. Coppa explained that many veterans, especially those just returning from service, don’t immediately have access to housing, and may be sleeping on couches with friends and family.
While it is hard to find data on the exact numbers of veterans facing mental health issues in New York City, the enormous numbers of veterans living in the area indicate that these problems identified on a national scale are going to be particularly evident here. City Council Speaker Christine Quinn testified at an oversight hearing on the high rate of suicide among veterans that it is likely that national trends of PTSD and other mental health issues are the same or higher in New York City. “This city is not the easiest place to live,” she noted.
PTSD can stem from other things besides direct combat experience. A factsheet issued by the Service Women’s Action Network (SWAN) says that while combat trauma is the leading cause of PTSD among men, military sexual assault is the leading cause ofPTSD among women veterans.
SWAN reports that 3,158 military sexual assaults were reported for 2010, with the Department of Defense (DOD) estimating that only 13.5% of sexual assault survivors report the attack. DOD estimates that in 2010 alone, there were more than 19,000 sexual assaults in the military.
PTSD is particularly likely in those veterans who served directly in combat, and in those most likely to have received abuses at the hands of others, including their command and fellow soldiers – women, non-heterosexuals, and people perceived to be non-heterosexual. For many sufferers the symptoms are manageable but difficult, hindering their health and happiness. For some, PTSD can be even more harmful, resulting in violence or injury to themselves or others.
Adding to the already-high incidence of depression among veterans is the difficult labor market they find on return. The Department of Labor estimates unemployment amongst Iraq and Afghanistan-era veterans to have reached a record 15.2% in January of 2011. Unemployment is a large and persistent stressor on individuals and their families.
The Veterans Administration
While the Veterans Administration is charged with making services available to veterans who enroll, many of those leaving the military do not receive the care they need from the VA. Reasons include a stigma associated with asking for help, as well as daunting enrollment procedures and a expectation of sub-par care.
SWAN National Peer Support Helpline Caseworker Rebekah Havrilla testified to the City Council that sexual assault survivors treated in military medical settings can experience further victimization, sometimes resulting increased rates of depression and PTSD. “I refrain as much as possible from referring female veterans to the VA.” she told the Council. SWAN’s website states that female sexual assault survivors report a lower quality of care from the VA than from outside care, and that there are “enormous barriers” to receiving VA disability compensation for sexual traumaâ€related PTSD, especially for women.
Coppa initially went to the VA for treatment for her PTSD. She said the crowds there are less of a problem than at city clinics, but long wait-times to be seen and a lack of privacy act as powerful deterrents, as does the lack of childcare accommodations. During a visit to seek help managing her flashbacks, Coppa was compelled to describe the most personal details of her trauma in a busy hospital, in front of her then-six-year-old daughter. “When we got back” Coppa recalled, “she begged me never to go to the VA again. It was such an awful experience.”
A Struggle to Stay
Asked how she will get the care she needs going forward, Selena laughs. “That’s a very good question. It’s not one I have an answer to.”
She hopes to be able to stay in Brooklyn near her family, but worries that the high cost of living and the lack of services may eventually drive her to move out of New York.
Despite her struggles, Coppa remains proud of her sacrifice for her country, and says she does not regret having enlisted.
“I still think it was the right thing, even though I don’t feel my service was valued – or is valued—by many. I still feel good about deciding to serve, whether or not I am served in return.”
Sex Education in the City
Photo by Romanna Klee
New York City will once again mandate sex education in public schools starting in the spring semester. It is not a moment too soon.
One of every four girls in the country between the ages of 15 and 19 has had a sexually transmitted infection, and 50 percent of black girls in that age group. In the city, teenagers account for one in four of all sexually transmitted infections. And while HIV diagnoses are going down in the city overall, they are going up among young men who have sex with men, especially blacks and Latinos according to Monica Sweeney, assistant commissioner at the New York City Department of Health and Mental Hygiene's Bureau of HIV/AIDS Prevention and Control. The department estimates that 4,000 people a year are becoming infected with HIV in New York.
The new mandate, announced this summer by Schools Chancellor Dennis Walcott, is part of the city's $127 million Young Men's Initiative targeting black and Latino young males through a combination of city money and private philanthropy, mostly from Mayor Michael Bloomberg himself and George Soros' Open Society Foundations.
"The chancellor and the mayor should be commended for implementing this new curriculum," said Michael A. Carrera, the dean of U.S. sex educators who began as a teacher in the Bronx in 1959 and has directed the Adolescent Sexuality and Pregnancy Prevention Programs at the Children's Aid Society since 1970.
He and other advocates, though, would like to see a program that is more comprehensive than what is being proposed.
While most city groups that work with adolescents fought for the mandate, opposition to it came swiftly from the Catholic Church. Joseph Zwilling, a spokesperson for the Archdiocese of New York, told the New York Times that the requirement "allows the public school system to substitute its beliefs and values for those of the parents." The Vatican newspaper featured an editorial condemning "useless, and even harmful, school courses."
Addressing a Need
In putting the new plan in the context of the Young Men's Initiative, the Department of Education is responding to the fact that 57 percent of new HIV diagnoses in the city in 2009 were among black and Latino men. They also saw that more than 40 percent of teens in East and Central Harlem, Bedford-Stuyvesant, Bushwick, and the South Bronx were sexually active versus a little less than 30 percent in the rest of the city.
While HIV is no longer a death sentence, those infected have to deal with a lifetime of taking medications and coping with their side effects. And sexually transmitted infections "make people who have them more likely to get HIV and more likely to infect others with HIV," Sweeney said.
While the new mandate made headlines, in the last school year 43 percent of high schools reported that they had already been using the high school version of "HealthSmart" and 38 percent "Reducing the Risk," two well-regarded and field-tested curricula. And in middle schools, 64 percent are using "HealthSmart" geared to those young people.
How We Got Here
It is not as if sex education is anything new in city schools.
A report prepared by NARAL Pro-Choice New York Foundation and the National Institute for Reproductive Health in November 2010 documents a history that began in the late 1930s. At that time, some Board of Education members, alarmed by high rates of pregnancy and sexually transmitted infections, called for "sex instruction, in the mild form of a study of mammalian reproduction." The proposal was rejected by the board, then endorsed by the United Parents Association in 1939.
It took until 1967 for the school system to offer "Family Living, Including Sex Education." Later that year, the state began requiring health education, including sex education -- though the sex education part was overturned in 1969. By the mid-1980s with the HIV/AIDS epidemic in full swing, sex education was still not reaching all students, so the state mandated AIDS education for middle and high school students in 1987.
In 1991 with AIDS raging out of control, people with AIDS dropping like flies, and no end in sight (this was before the mid-1990s advent of the drug combinations that vastly extended the lifespan of people with HIV), the New York City Board of Education enacted its own AIDS education mandate for all grades and made condoms available in high schools.
As director of education at the Hetrick-Martin Institute for LGBT youth then, I was -- full disclosure -- part of the AIDS Advisory Council to then Schools Chancellor Joseph Fernandez that wrote the 1991 plan and advocated for it. Fernandez put his chancellorship behind the plan and Mayor David Dinkins, who had two appointed two of the seven members of the board, expended significant political capital getting it passed.
After Rudy Giuliani became mayor in 1994, he gained influence over a majority of Board of Education members and encouraged them to ban condom lessons in classrooms and to enact a measure letting parents choose to have their kids opt out of the right to pick up condoms in high school resource rooms. Fernandez had resisted the latter as silly since a student barred from picking up a condom himself or herself could easily send a friend to get one.
Fernandez also stood behind multicultural curricula inclusive of sexual orientation issues, an issue that became a tabloid controversy when conservative Community School District 24 in Queens refused to implement such programs. When the board dumped Fernandez in 1993, the mainstream press often cited his role in these culture wars. In fact, his fractious relationship with the politicized board in the days before mayoral control was probably a more decisive factor. Nevertheless, for a decade city leaders were reluctant to stick their necks out on sex.
By 2003, Scott Stringer, then a member of the State Assembly, issued a report giving health education in the city schools a "failing grade." A push by a coalition of advocates got the city AIDS education curricula updated in 2005, revisions that I reviewed in Gay City News as light on dealing with the isolation of the young people most affected by HIV -- males having sex with males.
The election of a new mayor – Michael Bloomberg – with an interest in public health in charge, led in 2007 to the creation of the Office of Fitness and Health Education that recommended two curricula – "HealthSmart" for middle schools and "Reducing the Risk" for high schools. Until now, these were not mandated, but many principals opted to use them.
A poll sponsored by Family Planning Advocates in 2009 found that 85 percent of the New York State electorate supported comprehensive sex education in the schools and 77 percent believed – mistakenly -- that it was already mandated.
A diverse coalition of 30 groups cited that poll and a wealth of evidence on the need for a system-wide program in a May 2010 letter to then Chancellor Joel Klein. Earlier last year, the New York Civil Liberties Unions, a member of the coalition says it obtained "a previously unreleased evaluation of a Department of Education-approved, evidence-based sexuality education program that was piloted in 10 South Bronx middle and high schools during the spring semester of the 2007-2008 school year. According to the evaluation ... the pilot program was widely supported by teachers, principals, parents and students in the seven schools that completed it."
The New Plan
In introducing the Young Men's Initiative in an Aug. 9 letter to his colleagues, Walcott wrote, "We have students who are having sex before the age of 13; students who have had multiple sexual partners; and students who aren't protecting themselves against sexually transmitted diseases and HIV/AIDS. As a parent and a grandparent -- and as the person responsible for ensuring that all of our public school students receive a high-quality education -- that is very concerning."
All that is being required under the new plan is that schools offer "sex education lessons during one semester in both middle and high school." Teachers and principals have lots of flexibility about how to incorporate those lessons into the health curriculum and in which grade to offer the lessons. As with HIV prevention lessons, a parental opt out is being offered. Health educators will once again be permitted to demonstrate the proper use of a condom -- an exercise that teaches also opens a dialogue around how to negotiate for safer sex.
The city also is working on enhancing lessons relating to sexual orientation and gender identity and expression in the sex education curricula. This comes partly because the federal Centers for Disease Control is now pushing for such instruction in programs that it funds such as a five-year teen pregnancy reduction program in two Bronx community districts. And after decades of resistance to stepped up efforts to counter bullying, the Department of Education is spreading its "Respect for All" program throughout the schools. Under a new state anti-bullying law that soon kicks in, the schools will have to do even more in terms of tracking, addressing and preventing the problem.
The recommended sex education curricula are posted online for anyone to review: http://schools.nyc.gov/Academics/FitnessandHealth/StandardsCurriculum/default.htm.
The Next Steps
Alison Yager, supervising attorney for HIV Policy at HIV Law Project, is part of the Sex Education Alliance of New York City, a broad coalition that has long pushed for comprehensive sexual health education in New York City. She appreciates the city's move but think more needs to be done. She recently wrote wrote about the key role that HIV-positive women played in advocating for comprehensive sex education in New York City.
"We're thrilled that the city has taken this step," Yager said. "The question is: Will schools implement it, and if so, how? And further, how will the DOE and the public know what's happening in the classrooms?" Yager said that there needs to be "an enforcement mechanism and adequate oversight" of the mandate.
"The tremendous diversity among students in city schools creates another imperative,” Yager said. These lessons "need to be sensitive to students from varied cultural backgrounds, to both male and female students, and to be inclusive of LGBT students."
The Department of Education did not provide data on how well the existing mandates on HIV/AIDS lessons were being implemented, their effectiveness, the numbers of condoms distributed in high schools, or the numbers of parents who opt out of prevention lessons, though opt out rates for programs of this type in New York typically are below 2 percent of parents.
Edward Meachem, an attorney for the Catholic Archdiocese of New York, told the Times that he encouraged parents to opt out of any lessons involving contraception and to "inspect the materials to make sure there's nothing really offensive or inaccurate being put in there."
Margie Feinberg, a spokesperson for the Department of Education, said that the schools work with the Department of Health and other city agencies to "gauge how well we're doing" and is trying to pull together answers to the questions posed by Gotham Gazette.
Carrera wants to see more comprehensiveness and more integration in the city program, calling the new mandate "well-intentioned but strategically off."
"The focus of the initiative should not be pregnancy prevention, how to use a condom, HIV -- which are all important public health issues," he said. Instead, he said, classes should offer a more complete look at issues related to sexuality.
"The department," Carrera said, “missed an opportunity to comfort parents by telling them that this would be done in a more age- and stage-appropriate fashion that characterizes comprehensive sexuality programs in middle schools beginning with giving people information about puberty, their bodies, the bodies of others, gender roles, communication with parents, and essential messages about abstinence. The absence of that kind of presentation creates anxiety, causing parents to see it as having mainly to do with genital sexual contact."
Sexuality, according to Carrera said, should be taught weekly in middle and high schools. "It is as valuable as any academic subject. We are doing young people in public school a disservice by presenting this as short-term, fragmented exposure," he said. "It needs to be done in a thoughtful way."
Carrera said the experiences of the Children's Aid Society make it clear school can teach sexuality without alarming parents. Over the last five years, he said, the organization's programs have reached 1,500 students in a wide array of city regular public and charter schools, and no parent has opted out. His classes involve parents and provide instruction on sexuality in the context of an integrated program that also helps children get "no-cost medical and dental care in their neighborhood, on-site mental health services, and daily academic support. ... When we talk about comprehensive family living/sex education in that context it makes perfect sense to parents in the overall development of their child."
Carrera put forth his vision for Family Living Educator in 1993, and it has not changed. "The many fibers which comprise the fabric of an adolescent's sexuality suggest a holistic, dynamic definition of sexuality and sexual expression. If there is to be a new paradigm of adolescent sexual health, let it move from fragmentation to wholeness," he wrote then.
Melissa Goodman, the New York Civil Liberties Union's senior counsel for LGBT and reproductive rights emphasized that the city's Department of Education has to take steps to "ensure accountability and compliance" with the new mandate. "DOE should require regular reporting by schools and then publicly release evaluations of whether schools are complying with the mandate and how," she said. Her group hopes to "meet and work with DOE officials to discuss the new mandate and compliance with the HIV/AIDS education mandate."
Beyond that, Goodman said, the new program "needs to have explicit and clear requirements that schools teach a comprehensive range of topics that give students the information and skills they need to make healthy decisions throughout their lives" and "should address sexual orientation and gender myths and stereotypes."
Sweeney at the health department echoed the need for "multiple prevention strategies" to combat teen pregnancy and sexually transmitted infections, including HIV. "There is not one answer, one intervention. Parents need to talk about it with their children, religious leaders need to talk about it." Her department is funding peers – "youth ambassadors" -- who "talk to people in their own age group."
She also said we need to address the "structural issues" in the lives of young people, explaining "Kids who drop out are much more likely to engage" in risky activity. "We need all hands on deck," Sweeney said.
After Hurricane Irene blew through New York, the mayor was able to boast, "We didn't lose a single life." The city mobilized in an unprecedented way, shutting down the subway system for the first time and evacuating low-lying areas. It will take no less of a coordinated, comprehensive effort to bring teen pregnancy and sexually transmitted infection rates below the epidemic levels that they have reached. The quality and length of thousands of young lives are at stake.
Beyond Needle Exchange: Some Say Addicts Need a Safe Place to Inject

Photo by Todd Huffman
Bobby Tolbert is a slender, soft-spoken man with a wide smile and an understated elegance. He remembers when he began shooting heroin as a teenager in the 1960s.
"When I was coming up," he shakes his head, "we used a medicine dropper with a spike in it and a dollar bill wrapped up around it. We didn't have these syringes."
Tolbert grew up in the Queensbridge housing projects in Long Island City. At 15 years old Tolbert began what would be a multi-decade habit of use.
Back then, he says, no one thought there was anything wrong with sharing needles. But in 1995, after suffering a series of colds that wouldn't go away, Tolbert was diagnosed as HIV positive.
Tolbert sees his situation as fortunate. "I was one of the lucky ones," he said. "Eighty percent of those guys I used with are dead of HIV or overdose."
Tolbert's case is far from unique. Many injection-drug users continue to be at elevated risk, not only for HIV, but for other communicable diseases like hepatitis C, for overdose, for violence, and for other risk factors. These are serious health issues which affect not only the user, not only other users who might share needles, but potentially anyone using a public facility, walking down a city street, watching their child play on a public playground.
Under Mayor Michael Bloomberg, New York has done a lot to reach the somewhat paradoxical goal of improving the lives of people who shoot up drugs. But some advocates say the city could do even more -- finding inspiration in a new program in Canada that gives people a safe, clean place to inject their narcotics. Critics, though, say that creating such a service here would be politically difficult and detract from efforts to help people kick their habits.
Injection in the City
Despite advances, drug use still takes a heavy toll in New York.
The New York City Department of Health and Mental Hygiene calls New York City "the epicenter of HIV/AIDS in the U.S." It states that more than 107,000 New Yorkers are living with HIV and warns, "Thousands more don't know they're infected."
The department calculates that the AIDS case rate in New York City is almost three times the U.S. average and lists HIV as the third leading cause of death for New York City residents aged 35 to 54.
The statistics for New York state indicate that since the beginning of the outbreak, more HIV infections have been introduced through injection drug use than any other means of transmission. But in recent years, public health programs such as needle exchanges have had massive success in reducing the transmission rate in New York, and in 2010 a mere 4.3 percent of new HIV diagnoses were in people with a history of injection drug use.
There is still a long way to go, however. A 2008 study in the Harm Reduction Journal found that more than half of injection drug users were not able to consistently use sterile needles. And while syringe exchange programs help reduce the spread of HIV, they do much less to prevent transmission of hepatitis C, which can live not just in the needles but in the other equipment used -- and sometimes shared -- for injection, such as cotton balls, "cookers" or water used for cooking the drug.
Sean Barry, director of Voices Of Community Activists & Leaders, or VOCAL, a statewide organization serving low-income people living with and affected by HIV/AIDS, drug use and incarceration, said the success of reducing HIV transmission should not obscure the urgency of reducing other health risks associated with drug use.
"I think we now need to look at a more comprehensive approach to health. Not just HIV, HIV, HIV, which is what has been driving policy, but at other health issues, like overdose prevention and wound care," he said.
Overdose and Public Injection
A large factor in whether or not people use safer injection practices is whether or not they have a safe place to inject. People injecting in rushed, dimly lit, unclean or unsafe facilities are less likely to take the time to set up new clean equipment, and also far less likely to test a drug before injecting a full dose.
Public health leaders notes that users can reduce their risk of overdose if they test a drug before injecting it. Overdose is common in New York City, as different batches of the same substance can be cut with different ingredients and so can vary in strength and purity.
Barry points out that the danger of overdose increases when users inject drugs in places where users may not get help quickly.
"If people are injecting somewhere like a bathroom or a park, it's less likely that someone will notice if they overdose and their life is at risk," he said.
The Harm Reduction Journal study found that nearly half -- 49 percent -- of those studied reported injecting in a public or semi-public location in the previous month. This was particularly likely among people without permanent or private housing -- a significant percent of the drug using population.
Not only are injections in public places far more likely to be more dangerous to the user, they can subject other people in the area to risk as well from used needles and other detritus.
While the law requires that VOCAL inform anyone who comes into its office that drug use is illegal and so not allowed on the premises, the group also provides sharps containers in the bathrooms.
Barry said the goal is to try to ensure that, if people do inject, they will have a safe place to dispose of their needles. He calls that approach "reality-based," adding, "The reality is, people are going to inject drugs somewhere. So we can pretend it's not happening, but we know it's going on."
New York Gets Involved
Under Mayor Michael Bloomberg, Barry says, New York has taken a lot of step to lower HIV rates and address other issues with injection drug use. The City Council funded a coalition of groups called the "Injection Drug Users Health Alliance," which has allowed syringe exchange programs to scale up overdose prevention education and distribute Naloxone, a drug that counters overdose from opiate drugs.
While Barry said that the mayor has not directly funded any syringe exchange programs or other substance use programs around overdose prevention, he credits the department of health in this administration as being a very committed partner. "I don't think this issue was ever on Giuliani's radar, at least not in terms of implementing public health approaches," Barry said.
Barry also credits Bloomberg with sticking by public health decisions even when they are controversial, such as the safer heroin use pamphlet published by the health department that provoked sharp criticism from City Councilmember and Public Safety Committee Chair Peter Vallone and other officials.
Bloomberg, Barry said, "has really tried to remove politics from the equation, at least with drug user health."
Some policies predate this administration. Syringe exchange programs have operated legally in New York for 20 years, and the department of health publishes a needle exchange schedule on its website.
Barry says drug users want the tools to care for themselves and others. "There's a stereotype of drug users as selfish people, who don't care about the people around them or even about their own health, but it's not true. When people have access, they use it and take advantage of it. They don’t want to put themselves and others at risk," he said.
But needle exchange programs still face hurdles. Until recently it was illegal to possess a syringe with heroin residue in it, making people with dirty syringes to exchange vulnerable to arrest as they tried to do the safer thing.
Advocates were successful in changing the law so that people cannot be charged with possession for returning used syringes with a trace amount of heroin to a needle-exchange program. Yet many report that harassment continues. Tolbert says that it is not uncommon for overzealous police to tear up or confiscate the cards that identify people as participants in an exchange program, or to arrest people for loitering or trespassing now that they cannot make an arrest for syringe possession. He recalls one officer who described making arrests at a needle exchange program as "like shooting fish in a barrel."
Many syringe exchange programs do more than offer clean syringes. They clean up needle litter, maintain drop-in centers, and offer wrap around services and support such as housing, domestic abuse, medical, educational, or other help.
Safe Injection Sites
The program in Vancouver, British Columbia, though, goes a step further. Seven years ago, the city opened North America's only "safe injection site."
In an area once known to have the fastest growing HIV rate on the continent, drug users can now access medical testing and treatment, clean needles, counseling and security. The experiment seems to be working -- infection rates have fallen dramatically, overdose deaths have been prevented, needle litter has decreased, and advocates even claim that sexual extortion of addicts and overall neighborhood violence has diminished. Yet Insite remains the only such center in North America.
In New York, syringe exchange sites offer as part of their services judgement-free support for users in all parts of their lives, not just their drug use. At many programs, workers talk with recipients to identify and support their goals, and help user identify concrete steps towards accomplishing those goals.
Advocates say a safe injection site could provide these services and more. It could offer a safe, private place for people with addictions to engage in injection. This would be a tremendous benefit for the drug users, who can inject more safely in a clean facility with adequate light, medical professionals and sterile needles.
The benefit might be even greater to non-users in the neighborhood. Residents would be much less likely to witness -- or have their children witness -- injection. It would relieve non-professionals from the trauma and burden of trying to deal with people having bad reactions from drugs, and sharply minimize the risk of accidental contact with discarded needles. For users, a safe injection facility could be a place to seek counseling, treatment, or even just safety and understanding.
The Harm Reduction Journal concludes similarly. "Safe injecting facilities might resolve the syringe gap by attracting higher-risk injecting drug users, while reducing the public disorder caused by public injecting and relieving law enforcement of the effort required to address this problem."
"Is this another tool in the tool box to reach more people and save lives? Without a doubt, yes," Barry said.
Barry says safe injection sites cannot even be discussed in New York without immediate controversy, but he believes that could change. He points to a history of support on the state level for public health measures. Gov. Andrew Cuomo recently signed the Good Samaritan law to prevent arrest of people who call emergency services to report an overdose, and his predecessor, Gov. David Paterson signed a law to prevent the arrests of people participating in a syringe program.
"I can see Bloomberg and his administration finding some way to explore this," Barry says, referring to a safe injection site, "But I don't think he is going to do it without a strong push from advocates."
Some, though, think such an effort would detract from what should be the primary goal: getting people off drugs. City Councilmember Charles Barron of Brooklyn agrees with VOCAL that drug response policy should change from a criminal approach to one of public health, but he calls the philosophy behind safe injection sites "defeatist" and says he would oppose such sites opening.
"That's just maintaining them shooting death in their veins instead of helping them to get off the drugs," Barron said. "That doesn't make any sense."
Barron said, personal opposition aside, he does not think such an effort would survive politically. "I don’t see it taking off," he said.
Sites identified as potential locations for such a service include parts of the Bronx, East New York in Brooklyn, Harlem in Manhattan and parts of Queens. Caseworker Christina Ann with the East Harlem Neighborhood Alliance says she believes some of these communities might be open to a safe injection site. "I'm sure it would be welcome in the neighborhood," she said.
However not everybody is so sure. Matthew Washington, chairman of East Harlem's Community Board 11, takes issue with the idea of that neighborhood becoming a possible location for a service for drug users. "Dealing with injection drug use is something that everybody needs to deal with, and something the city needs to address collectively," he said. "But the city is unequally dumping these sorts of facilities in our community."
'There But For the Grace of God'
The HIV diagnosis changed life for Tolbert. Today, he works as a peer educator, teaching other injection drug users about the importance of safer injecting. He is a tireless advocate, working on issues like affordable housing for HIV positive people, and serves on the board of VOCAL.
He volunteers at needle exchange programs, and spends time going into SROs to talk to people living in poor conditions like the ones he used to live in.
"I try to educate people on how to get out of that situation, because there but for the grace of god go I," he explained.
In May Tolbert will be the keynote speaker at the Harm Reduction Coalition conference in Washington D.C.
"Now that's all I do," he laughs. "All I do is educate."
Citing 'Emergency,' Council Passes Animal Bill

Photo by Shavon McKinstry
The New York City Council yesterday passed a bill that would extend hours at animal rescue centers, seek to reduce the number of feral cats prowling city streets and increase the budget for animal services in the five boroughs.
Yet while many animal rights groups applauded the measure, other organizations and some elected officials condemned it as a ploy to relieve the city of having to provide additional services and of possibly losing a lawsuit challenging its treatment of animals. As evidence, these advocates charged the City Council had rushed the bill through, holding hearings last week and passing it today.
City Council Speaker Christine Quinn said the bill had been in the works for about nine months. The council decided to act today, she and the measure's author, Manhattan Councilmember Jessica Lappin said, because animals in the city face an emergency.
On that point, it seems, few disagree.
The Council Bill
The measure, Intro 655, which passed 46 to 4, has a number of provisions.
It would expand the hours at centers in the Bronx and Queens where people can drop off stray and lost animals. In those two boroughs, the center currently are open only several hours a week. They will now accept animals for 12 hours a day seven days a week.
The bill also substantially expands the hours when field services will go out and pick up injured or otherwise distressed animals.
In an effort to reduce the number of feral cats throughout the city, the measure requires owners to spay or neuter cats they allow to roam free and seeks to strengthen trap-neuter-return, in which groups or individuals collect feral cats and neuter, vaccinate and identify them before returning the animals to the streets. The health department will issue rules requiring registration of anyone who treats the animals. "We want to make sure people really know how to do it, are trained how to do it," Quinn said.
While the aim of these initiatives over the long term, said Jane Hoffman, president of the Mayors Alliance for NYC's Animals, is to "reduce and eventually eliminate cats outdoors," in the interim "what you need to do is give them a good life and treat them humanely."
The bill requires the Department of Health and Mental Hygiene step up its monitoring of Animal Care and Control, the much maligned nonprofit that runs the animal shelter system. And it increases funding as well, with a extra $1 million this fiscal year and a hike of 77 percent -- to $12 million -- by 2014. In an effort to attract additional private funding, the bill also adds two more members of the public to the Animal Care and Control board.
Together, Lappin said, "This will really improve the services on the ground in the Bronx, Queens and all five boroughs."
A number of animal rights groups, agreed issuing statements in support of the measure.
"In these tough fiscal times, access to increased monies for programs and services that have been stretched so thin is a welcome change," Hoffman said in a statement issued by several of the groups. "Providing this infusion of critical resources will help save lives and prevent animal suffering."
Too Little, Too Soon
Even the four council members who voted against the measure did not disagree with that. The problem, critics said, is that the bill does not do enough to repair what they see as a severely flawed system a system that shortchanges the Bronx and Queens.
Much of the controversy goes back to 2000 when the City Council passed a bill requiring a full-service shelters in each of the boroughs. Neither the Giuliani nor the Bloomberg administrations complied with that, a failing Quinn attributed to the difficulty of finding appropriate space for the facilities.
In 2009, the group Stray from the Heart filed suit accusing the city of violating the law. The advocates won in the trial court, but an appeals court ruled the group did not have standing to challenge the city on this. Then earlier this month, the Court of Appeals agreed to hear the suit.
The bill passed yesterday would no longer require the full-service shelters in all boroughs. The service centers it discusses do not have veterinarians on staff. Calling the bill "a wolf masquerading in sheep's closing," Laurie Bleier of Brooklyn Animal Foster Network, said it will do nothing to get a vet to a dog hit by a car in the Bronx or to provide medication to an abused dog in Queens.
By acting now, some critics said, the council let the city off the hook in the event of any legal ruling against it.
"I don’t think you have to be smarter than Bonzo the chimp to figure out what's going on," City Councilmember Peter Vallone, who voted against the bill, said before the meeting.
Later, speaking in chambers, he said, "This bill insures the people in Queens and the Bronx won't have a full-service shelter. It may rain cats and dog before they have that shelter."
In a statement, Ed Sayres, president and CEO of the ASPCA denied the measure would prevent the establishment of more full-service shelters.
"We cannot stand by and let animals suffer in our city," he said. "Intro 655 is an immediate solution in the midst of this crisis. We absolutely believe that there must be animal shelters in all five borough but we need urgent support now."
Show Them the Money
Critics also worry the promised $12 million never will materialize.
As he explained his no vote, City Councilmember Dan Halloran raised that concern. "There is a problem in City Hall in keeping the promises it makes to this body in budget negotiations," he said. "I hope the city's animals will not pay the price."
Quinn acknowledged there were no guarantees. "All you can do with any budget is make sure the money is in there one year at a time," she said.
Michelle Villagomez, a spokesperson for the ASPCA, said the funding was needed. "New York City Animal Care and Control has experienced budget cuts, she said, that have had an effect on staff and services and forced it to "make reductions in day to day care." The additional money, she said, will improve care of animals, increase the likelihood of animals being adopted and expand services in the outer boroughs.
Underlying much of the debate on both sides is a general discontent with Animal Care and Control and with city funding for animal services. "You’re giving $10 million to one of the most mismanaged board of directors," Zelda Penzel of S.O.S. Save Our Shelter Animals said. "It’s a total sham."
Councilmember Vincent Ignizio, who said he originally planned to vote against the measure but changed his mind, chastised the Bloomberg administration "for allowing the state of repair of ACC to fall so low."
Councilmember Leroy Comrie complained the agency had repeatedly failed to respond to complaints about packs of wild dogs in his district.
Recently Manhattan Borough President Scott Stringer has called for a total revamping of Animal Care and Control. "There are inhumane conditions. There are healthy animals being put down, animals sleeping in their own waste," Stringer http://ourtownny.com/2011/09/21/who-will-save-them/tolf Out Town. "We have members of the board who have absolutely no experience in fundraising and no experience in animal control. It's a disgrace."
Stringer, according to the paper, has proposed that Animal Care and Control be made a quasi-independent agency like the Central Park Conservancy.
Quinn acknowledged concerns about Animal Care and Control resources and performance. Even with the increase in funding, she said, "When you compare it to other cities, it is not really the amount of money that we need."
As for the job the agency has done, she told her fellow council member, "We're not going to take Animal Care and Control at its word. … For some time it hasn’t been up to its mission."
Putting Housing Inspectors on the Guards

Photo by dghilli
With the budget passed and the summer over, the City Council yesterday got returned to its regular schedule. But while the fall usually brings a spate of legislation -- a fraction of which even sparks controversy -- Tuesday's meeting brought unanimous votes on the only two bills under consideration.
The highest emotion came in comments on an item not on the council agenda: the detention by police Monday of one of the council's members -- Jumaane Williams -- and a political aide.
Several council member stood to declare their support for Williams and to call for the changes in police procuedres that several said had lead to the handcuffing of the two black men -- and to the stops of hundreds of black and Latino men every day.
Putting Their Guard Up
In what City Council Speaker Chirstne Quinncalled an efort to make better use of city resoures, the council approved Intro 531-A, which would step up enforcement of city rules requiring that all apartments occuped by young children have guards on the window.
Currently, only health inspectors have the authority to check for window guards. The bill would also allow housing inspectors to check for the window guards and to order owners to install them where needed. Owners who do not coply within 21 days face fines.
Empghasizing the measure does not take any authority away from the health department, Quin said it "also gives that power to housing inspectors who are out there every day."
In the city, Quin said, "The number of children who fall out of windows is not as high as it was at one time," but national figures indicate the need to make sure that window guards are in place.
Cleaner Waters
The council also approved a measure aimed at cleaning up the city's 520 miles of shoreline and its waters by requiring the Department of Environmental Protection, Department of Sanitation and Department of Small Busines Servies to coordinate efforts to combat illegal dumping. The agencies also would also have to report on the implementation of the plan.
Speaking next to a photograph of tires dumped on the shore, Quinn said the city has not had a unified effort to prevent dumping and the efforts of various agencies have been "sporadic at best and clearly inadeuqate."
A Taskforce on Violence
Before the meeting -- and after a weekend marked by a rash of gun violence cross the city -- Quinn announced the council had formed a taskforce on gun violence to be chaired by Williams and Councilmember Fernando Cabrera. Acording to the announcement, the committee, which will focus on black and Latino communities, will look at the causes of the violence and look at ways the city could help combat it.
As an example Quinn cited a campaign in 2008 to fight back at the taboo on snitching in some neighborhoods.. The city covered graffiti condeming snitching, she said, and "we began to send a message that it's not snitching, it's saving a life."
Quinn conceded that at least some of the problem lay not in the city, but with lax gun laws in other parts of the country. While supporting the push for tougher gun laws nationally, she said, "We are also going to find ways to do what we can locally."
Fight Over Compensation for 9/11 Responders Shifts to Cancer Victims
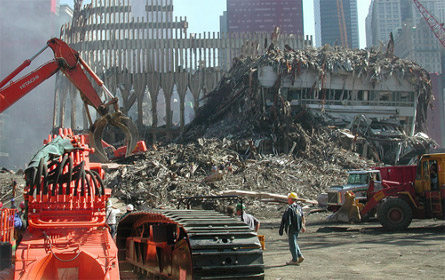
Photo by Matt Morgan
Responders worked to collect remains and clear debris for months after the trade center fell.
"The Tea Party hasn't dealt with John Feal yet," said John Feal, the former construction worker who has been one of the loudest advocates for sick and injured 9/11 rescue and response workers. Missing half a foot as result of his efforts at Ground Zero, Feal often stands out among the politicians and union officials who speak in diplomatic, politically safe terms.
Feal was referring to his movement's latest hurdle: amending the James Zadroga Act -- a bill passed last year ensuring federal funding for 9/11 health monitoring and treatment programs -- to cover certain types of cancers. In July, the federal government announced the bill would not provide medical benefits to first responders who developed cancer. Now the unions and other hope a new report will make their task easier.
Difficult Politics
Even with a Democratic Congress and the help of the New York and New Jersey congressional delegations, passing the Zadroga bill at all turned into a Sisyphean task in the face of fierce Republican opposition. After a series of compromises, Congress finally approved it last year after what New York Sen. Kirsten Gillibrand called a "Christmas miracle."
The problem is not only that the House of Representatives has fallen into Republican control since then, but that the hard-line Tea Party caucus has proved it will adamantly oppose almost any increase in federal spending. Standing for thrift instead of helping first responders becomes more mainstream with each passing year since 9/11.
Even in the five boroughs, criticizing the Zadroga bill -- named for a New York police detective who died from what many believed were 9/11 related-illnesses -- is no longer political suicide. Bob Turner, the Republican running for the House seat vacated by Anthony Weiner, said the bill was "too broad" because it covered of volunteers. He has the endorsements of former mayors Ed Koch and Rudy Giuliani, as well as Long Island Rep. Peter King, a Republican credited with fighting opposition to the bill in his party.
A Fight Over Evidence
In announcing their decision not to cover cancer victims, federal officials said no solid evidence existed linking the cancers to exposure to the toxins found at the former World Trade Center site.
The reportby the National Institute of Occupational Safety and Health, though, also said that there was no evidence that a link did not exist. Trying to prove things one way or the other, the institute said, presents a challenge because there are few published studies on the issue- - and even fewer that were peer-reviewed -- and because cancer is "not a rare disease."
The federal government expects to review the issue again in the middle of next year.
Last week, though, responders got a boost when The Lancet released a study that, the New York Times reported, "says firefighters who toiled in the wreckage of the World Trade Center in 2001 were 19 percent more likely to develop cancer than those who were not there."
The Lancet reported it found "a modest excess of cancer cases" in those who were at the trade center site. It said it remains cautious about the findings because of the short time since the 9/11 attacks and because the increase is not confined to any particular type of cancer.
Feal, though, dismissed such hesitancy. "I don't need a doctor or a scientist to tell me that 9/11 caused cancer," he said. "We see the pain and suffering every day and we expect with this study that cancer be added to the bill in an expedited manner."
Union leaders like Uniformed Firefighters Association President Steve Cassidy have noted in the past that responders under the age of 40 have already developed cancers, even though the initial reports said they would take at least 10 years after 9/11 to occur.

Photo by Marion Doss
Three days after the attacks, a firefighter wipes soot from his eye at the World Trade Center site.
"Cancer is the quintessential disease," Feal said, noting that these types of cancers are either hereditary or caused by carcinogens. "We have the statistics and the numbers, and they can't deny it."
Last week, the federal government announced one expansion of the program – extending it to people who lived and worked south of Canal Street. Originally the compensation only applied to people who had been south of Reade Street, about 10 blocks farther south.
Evidence suggests "that prolonged exposure to dust between Reade and Canal streets created a demonstrable risk of physical harm," said Sheila Birnbaum, head of the Sept. 11 Victim Compensation Fund.
At the same time she ruled out extending benefits to cancer victims, at least for now.
Hurdles Along the Way
On the one hand, implementation of the Zadroga act is working well, according to advocates, both in terms of ensuring that the 9/11 health centers can operate without the distraction of operating on annual appropriations and in allowing sick responders to seek compensation.
"They're not looking over their shoulder any more," Feal said of health providers. "Everything is up and running smoothly. That's a bonus. The compensation part is going to start in October. We're on track. Everything we've predicted in the past is coming to fruition."
But getting to this point has been a political drama. First, the city’s chief medical examiner claimed that Zadroga had, in fact, not died of 9/11 illnesses but from prescription drug abuse. While this didn’t directly affect the proposed legislation, it damped his name’s significance.
In late 2008, Congress delayed voting on the bill to attend to the emerging financial crisis. And when a Democratic House seemed to ready to pass the bill, it used a rare parliamentary procedure to block voting on Republican amendments to the bill, in particular one that would bar undocumented immigrants from benefiting from the law. That maneuver meant the bill needed a super-majority to pass, rather than 50 percent plus one, effectively killing it at the time.
The bill finally did come through last year with some compromises on funding, but Republicans demanded language that required that all recipients of Zadroga bill aid be checked against the terrorist watch list. The screening found no terrorist suspects seeking aid.
"They made this big deal about nothing," said Bill Henning, the chairman of the New York Committee for Occupational Safety and Health. "It was just so insulting."
Beyond helping those disabled by their time on "the pile," union officials and health advocates hope the information that comes out of the compensation fund can help future workers. On Sept.16, the New York Committee on Occupational Safety and Health will hold a conference titled "Protecting Worker and Community Health: Are We Prepared for the Next 9/11?" with speakers including World Trade Center Health Program director John Howard and Occupational Safety and Health Administration chief David Michaels. The reason so many workers are sick now, advocates say, is that the city did not provide adequate masks to protect responders from the toxic soup at Ground Zero. They also claim that the U.S. Environmental Protection Agency at the time made overly optimistic statements about the air being safe to breath.
As Feal noted, the current state of health care for the workers might be adequate, but it has been a struggle to get Congress to commit the federal government to funding these programs.
"We lose a lot of good people in every battle we have to face: a firefighter, a cop, a construction worker," Feal said of the responders who have died in the meantime. "It's a shame that they don't get to see the good."





