Senate Republicans in No Rush on Health Insurance Exchange

As the legislative session came to its end in June -- the Capitol shaking with the chanting of protestors for and against same-sex marriage -- numerous pieces of controversial legislation also were settled and voted on. But when the emotional vote on gay marriage ended, Senate Majority Leader Dean Skelos called an end to the 2011 legislative session, leaving some lobbyists and lawmakers shocked.
Observers weren't surprised that the Senate failed to take action on controversial bills such as independent redistricting, but one piece of legislation remained that had been agreed to by the Assembly, governor and Senate -- legislation that would see the creation of a federally mandated health insurance exchange.
Under federal health care reform law, every state must set up a one or more health insurance exchanges to help provide heath coverage to residents who are not insured through their jobs. When the Senate left town without acting on the insurance exchange legislation that was passed by the Assembly, it missed the first deadline. Even though New York lacks a plan, Washington still provided the state with funding to set up an exchange.
Health care experts, though, question how long Washington will maintain its generosity. And they caution that, funding issues aside, the state needs to get to work on the very complicated task of laying the groundwork for its exchanges or risk being forced to accept a federal plan that may not be to its liking.
Questions of Timing
The legislature and governor reportedly agreed on a bill in June. While there were numerous versions of the bill, the one they concurred on was a slightly altered version of a bill put forward by Senate Republican health committee chair Sen. Kemp Hannon. S.5849, the New York Health Benefit Exchange Act, would create the exchange as a public benefit corporation with nine unpaid directors, seven of them gubernatorial appointees and two legislative. The bill left several technical issues unresolved such as how to finance certain benefits, but set an April 1, 2012 deadline to resolve them.
Some Republicans felt reluctant to go on record in support of "Obamacare." The decision to bring same-sex marriage to a vote was enough of a strain on some members that they refused to vote on the legislation -- despite the deal with Cuomo and the Assembly.
On a policy level, some members have distinct concerns about the effect a health care exchange will have on small business. Consumer groups want to maintain strict controls on what kind of plans can be offered, while small business groups want to make sure there is a wealth of options because of cost concerns.
Advocates of the legislation assumed that the Senate would return this summer or fall to approve labor contracts and vote on health care exchange legislation, but as the summer wore on more Republicans made it clear they felt no pressure to vote on the legislation.
Now it remains unclear what the Senate will do.
"The basic answer is I don't know," Hannon told the Gazette this week. A spokesman for Skelos said that there are no plans to return to Albany. "We do not currently have any plans to return," said the spokesman.
Hannon said that he thinks the agreed-on bill could be renegotiated and points out that he and his colleagues don't feel much pressure to move on the legislation when the federal government is sending the state money even though it missed the June 30 deadline to pass legislation.
In fact, New York has received three grants from the federal government specifically for the construction of an exchange: a $1 million grant for exchange planning to the Insurance Department, a $27,431,432 Early Innovator grant to the Health Department and a Level 1 Exchange Planning Grant worth $10,774,898.
And Hannon said that a great number of otherwise uninsured New Yorkers are, "already on Medicaid."
Elisabeth Benjamin, vice president of health initiatives for the Community Service Society, was fairly upbeat about the prospects of legislators to returning this fall to vote on the exchange legislation. But when told about Hannon's comments she seemed a bit exasperated.
"Applying for federal funding is not as simple as sitting down at your computer terminal one morning," she said. “You have to set up an agency, have to have a director, a plan, a staff before you apply for level 2."
Benjamin further explained that the agency would have to decide what kind of coverage it would offer, how it will offer the plans, if the plans will be standardized, what roles brokers would have and a whole other list of specifics.
Once the election year begins, the prospects of getting a bill through would grow dimmer. "If you think you can pass the bill in 2012 ... that is just insane," said Benjamin.
New York is supposed to have an exchange up and running and certified by the federal government by Jan. 1, 2013, or face intervention by federal authorities.
If it fails to set up its own exchange, Benjamin said, New York will leave itself at the mercy of the federal government. "The people who are so afraid of 'Obamacare' -- that is exactly what they will get if they don't get the exchange in place. The feds will come in and do what they want. They will set something up that doesn’t use our agencies and doesn’t have our consumer protections."
Running Behind
But New York is not alone in being behind schedule in setting up an exchange, and federal officials have acknowledged that. Fewer than a dozen states have implemented exchange laws, and the lawsuit against health care reform has kept some Republican states from acting.


Steve Larsen, deputy administrator and director of the Center for Consumer Information and Insurance Oversight which is an arm of the federal Centers For Medicare and Medicaid Services, announced rules in late July that would make the deadline flexible. The rules would allow states to have part of an exchange active by 2014 with the federal government filling in the what the state was not prepared to provide. States that missed the deadline all together could apply to create an exchange later on. The Center for Consumer Information and Insurance did not return calls for comment.


Despite possible changes at the federal level, Sen. Neil Breslin, the ranking Democrat on the Senate insurance committee, said he is concerned that, if New York does not act, it will miss out on funding. "Federal money is available on a first come first serve basis. There are two monies available -- to create an exchange and to sustain it," he said.
While New York has received phase 1 grants without meeting phase 1 requirements, Breslin does not think that will continue through phase 2. And if New York misses the deadline all together, Breslin said, "Then we don’t determine what we want to do, the federal government implements something and charges us for it. The insurance department is very concerned."
Benjamin agrees the state will lose money if the Senate does not act. "Yes, they are getting some money, but they can miss out on so much more. We could get enough money to run the entire exchange," she said. But for that to happen, she said, "We have to have a certified functional exchange by 2013 ... . You can't just pass something in 2012 -- there won't be enough time. This isn’t a simple thing."
In Cuomo's Court
So what could change things? What could get Senate Republicans back to Albany to vote on the agreed-upon exchange legislation?
The same thing that makes everything else happen in Albany these days: Gov. Andrew Cuomo.
"The governor has to be the ultimate advocate for New York to step up and have a functional health insurance exchange. The governor did a good job negotiating a three way bill, now he has to get them to pass it," says Benjamin.
Benjamin said she is certain legislators are well aware of the bill and the time constraints. "This is not off their radar. They are getting memorandums of support and letters in their mailboxes everyday. Unless they don't check their mail."
Cuomo has remained silent on the topic. His office did not respond to calls for comment. Some Democrats think Republicans are avoiding a return to Albany so as not to face pressure on independent redistricting and that the governor has decided the exchange is not a priority.
That could change if members of the Public Employee Federation vote to ratify their new contract. Then the legislature would likely have to return to approve the pact. Once the members are in Albany anyway, the Assembly could ask Cuomo why he is not pressing the Senate to vote on a bill that has already been agreed upon.
Hannon does not seem to be in any hurry. "It's not certain their will be a special session," he said. "The governor may like us, but I don't know if he wants us back that badly. This could be addressed next year. The important thing is we get the right system."
St. Vincent's Highlights Crunch for Hospitals Serving the Poor

The area around 12th Street and Seventh Avenue in the heart of Greenwich Village is remarkably quite these days -- so quiet that Yetta Kurland, an activist, goes so far as to say that "it almost looks like a bomb went off."
The block was home to St. Vincent's Hospital Manhattan, which closed in April 2010 after years of financial troubles. St. Vincent's, which cared for victims of the Titanic, the AIDS epidemic and the 9/11 attacks, was New York City's last Catholic general hospital, and its absence has been felt throughout the community.
In addition, St. Vincent's was one of New York City's most prominent safety-net hospitals, serving mostly those either on Medicaid or Medicare or without insurance. It was also known as a refuge for the homeless. It has principally been these patients, then, who have been hit the hardest by St. Vincent's closing and by the shutting of other hospitals elsewhere in the city.
Filling the Void
Regardless of income, most residents of the Lower West Side who used to go to St. Vincent's now end up either at Beth Israel or Bellevue on the East Side. Shortly after St. Vincent's closed, Timothy Lunsford, a survivor of two heart attacks and two bouts of cancer, experienced a medical emergency in which his blood pressure dropped to a dangerously low level.

"It took me 33 minutes to get from Canal Street and Varick to Beth Israel hospital," he said.
Both hospitals have had to adapt to a rapidly growing patient volume, which Lewis Goldfrank, Bellevue's chief of emergency medicine, has called "a significant disaster."
"Those 60,000 people [treated each year at St. Vincent's] now have to find another place to go, so the nearest emergency rooms are overwhelmed. … And it's not because the hospitals aren’t trying, but they're unable to cope with what is a disaster," said David Kaufman, a member of St. Vincent's medical staff for 30 years and a part of the Coalition for a New Village Hospital.
With no access to local care, overcrowded emergency rooms in neighboring hospitals, the loss of a medical safety net and longer waits, the health situation in Greenwich Village is a "crisis," according to Kurland, also a member of the coalition. To remedy the problem, the coalition wants to see nothing less than a full-service hospital at the former St. Vincent's site.
Not Quite a Hospital
The plan reached by Rudin Management, a development firm, and North Shore-Long Island Jewish Health System does not align with that vision. (Disclosure: My father is a doctor at Lenox Hill Hospital, a member of the North Shore network). Instead, it would create 300 luxury apartments and townhouses on the eastern side of the medical campus and refurnish the historic O'Toole buildinginto a freestanding emergency department to be operated by North Shore.
The ability of the care center to serve the 385,000 New Yorkers living in the Lower West Side remains hotly contested. According to Terry Lynam, a spokesperson for North Shore, the care center will be able to treat 90 percent of patients. "[It] would be the same kind of emergency department you would see in most hospitals with the exception that it doesn't have inpatient beds," Lynam said.
The facility would provide around-the-clock diagnosis and treatment services. It should also be open to those on Medicare or Medicaid.
However, since it would not have the resources of a full-service hospital, including operating rooms and an intensive care unit, patients suffering from heart attack, stroke or major trauma would "need to be transferred elsewhere," Lynam said. She emphasized that agreements will be in place with local ambulance providers so they do not bring these patients to the care center in the first place.
Kaufman, however, argued that these restrictions will "create a life-threatening sense of confusion for patients and ambulance drivers."
If an emergency patient does enter the care center, the amount of time it would take to transfer him or her could prove significant, according to a recent study by the Journal of the American Medical Association. It found that it takes nine out of ten transferred heart attack victims more than 30 minutes to reach their second facility, above the recommended medical guidelines. These patients consequently suffer higher mortality rates.
Despite this proviso for emergency cases, Lynam said the care center "is returning health care to the Village" and "will save lives."
But coalition members remain unconvinced. Kaufman in particular worries that the care center will be unable to manage the large number of patients who used to enter St. Vincent’s doors.
"Can their comprehensive care center … treat 61,394 people a year?" Kaufman asked at a rally on April 30. "Can it house 19,388 patients sick enough to require inpatient care, can it deliver the lifesaving, critical care that 13,572 poor souls required in the emergency room in 2009?"
Recipe for Failure
Others, though, look to the closing of St. Vincent's and see a lesson for anyone thinking about opening a new full-service hospital in the area. St. Vincent's failed after a decade of mismanagement, including a hospital merger in 2000 and the hiring of consulting firm Speltz & Weis in 2005.
St. Vincent's failure, though, also speaks to a troublesome citywide trend for charity hospitals -- a trend that has severe implications for low-income communities. Following the tradition of the Sisters of Charity, St. Vincent's was dedicated to "compassionate care": serving the poor and disenfranchised. Like many other struggling safety-net hospitals, St. Vincent’s charitable mission, ill-suited for today’s high-tech, costly health care, led to its end.
Over the last ten years, the state's Medicaid reimbursements, a significant portion of St. Vincent’s revenue, have been cut. Moreover, while St. Vincent's saw an increase in emergency room visits, which are costly and in many cases go unreimbursed, its inpatient volume decreased as wealthy residents left for more prestigious institutions.
In general, New York City hospitals are struggling. Over the past decade, hospitals nationwide have seen average profits of 4 percent, whereas in 2008, hospitals in New York City faced an average 6 percent loss.
Since deregulation in the 1990s, safety-net hospitals have struggled with less government support. What was once a highly regulated industry became a free-for-all, as "suddenly hospitals were put in the position of competing with each other," North Shore's Lynman said. This took a toll in New York City where hospitals are located close to one another, the most noticeable example being New York Presbyterian-Cornell Weill, Mount Sinai and Lenox Hill all on the Upper East Side. Without state regulation, this competition allows insurers to drive down reimbursement rates, fueling hospital debt.
To stay economically viable, hospitals vie for privately insured patients, setting off what has been called a medical technology "arms race" that raises the price of health care. They are far less eager to take in publically insured -- or worse yet, uninsured -- patients. In New York, reimbursements by the public insurers Medicare and Medicaid are notoriously low. This means that those on public insurance or not insured at all—the majority of St. Vincent's patients— place a financial burden on struggling institutions.
Evidence of the strain abounds. In 2009, in the wake of the H1N1, or swine flu, outbreak, Mary Immaculate and St. Johns – both safety net hospitals in Queens -- closed. According to a 2009 report from former City Comptroller William Thompson Jr., this led to "overcrowded emergency rooms, longer wait times for patients, and longer ambulance turnaround times."
Jamaica Hospital has picked up a flood of Mary Immaculate's and St. Johns' patients. Its emergency room, built to accommodate 60,000 patients annually, now sees 131,000. Emergency care is costly to provide, and in 2009 Jamaica Hospital lost $13.5 million. If Jamaica, one of the borough’s most prominent safety-net hospitals, goes the way of Mary Immaculate and St. Johns, the health implications, particularly for poorer residents, could be devastating.
This is a familiar pattern. When safety net hospitals close, low-income, already underserved communities bear the brunt of the impact. Patients spill over to surrounding hospitals, overcrowding their waiting rooms and increasing their financial pressures, setting off what could become a chain of hospital failures.
In the case of St. Vincent’s, Bellevue has absorbed much of the excess patient volume both because of its relative proximity and the fact that it is now the only Level One Trauma Center in lower Manhattan. Bellevue now serves an additional 2,000 people each month in its emergency room, a 25 percent increase. Beth Israel has also seen a 25 percent traffic increase with slightly higher numbers these past two months.
"What happened last year was not a tsunami that came and went, but the increase has been sustained," said Gregg Husk, chairman of the Department of Emergency Medicine at Beth Israel. Beth Israel has increased its emergency room personnel, nursing staff and physicians and recruited former St. Vincent's programs, such as the Comprehensive Cancer Center.
Beth Israel is still "tweaking" some of its health care practices to adapt to the increased patient volume, but overall, Husk said, "we were very fortunate" and "the environment is not chaotic."
Despite this, a June 2011 study on St. Vincent's closing wrote that the surge of patients to neighboring hospitals "was characterized as 'crushing' to staff morale as hours and workload increased dramatically." The study also reported patient crowding and increased waiting room violence.
The trend toward deregulation leaves little hope low-income New Yorkers will regain their safety net care in the future. "The changing landscape of healthcare is such that no one in the New York City area is building new hospitals," said Lynam.
Counting Beds
After St. Vincent's closed, Rudin Management proposed to donate the O’Toole building and $10 million in funds for an urgent care center run by North Shore. In April 2011, a bankruptcy court judge approved the transaction.
"This is the only deal that is doable in today's environment," said John Gilbert, executive vice president and chief operating officer for Rudin Management.
Mount Sinai had been prepared to take over and run a full-service hospital in the neighborhood but suddenly withdrew in April 2010. Coalition members blame this on a lack of support from the state Department of Health which, following the recommendations of the 2006 Berger Commission, is trying to limit "the state's unacceptably high excess capacity of hospital beds."
The North Shore care center will not create any new impatient beds and so aligns with the state's goal. A new full-service hospital on the other hand would work directly against it.
The coalition argues the focus on overall number of beds is short-sighted. "They give no thought to the distribution of beds -- all they care about is shutting them down. Community needs, bed per person ratios, socio-economic issues are all irrelevant," said Kaufman at a rally in April.
Kaufman has pointed out that in the Upper East Side and East Harlem there is one bed for every 82 residents. In contrast, after St. Vincent’s closing, there are now no hospital beds for the West Side’s 385,000 residents.
Judy Wessler, director of the Commission on the Public's Health System, noted that hospitals in New York City have "always been mal-distributed," but with the closing of many charity hospitals in underserved communities, "it's getting worse."
"The East Side is wealthier, and that's where institutions tend to settle," she said. "Studies have [shown] over and over … that there is an absolute correlation between income and access to health care and even race … and access to care."
The coalition continues to fight the Rudin/North Shore plan. Yet, while it has galvanized support among community members, it has failed to win backing from some key politicians and other community leaders. Councilmember Christine Quinn, former Mayor Ed Koch and Greenwich-Chelsea Chamber of Commerce president Tony Juliano have all spoken out in favor of the comprehensive care center.
"Our health care needs are significantly underserved. This will go a long way to bring this service back to the community,” said Juliano, warning that if the community does not support the North Shore plan "we'll be looking a year from now … at a horrible situation where a whole city block is vacant."
Since St. Vincent's declared bankruptcy in 2010, 3,500 former employees are jobless and around 40 local businesses have closed. Juliano hopes the development will "bring economic life back" to the neighborhood.
Proponents for the Rudin/North Shore plan argue that, while it may not be ideal, it represent a pragmatic solution to an admittedly bad situation.
"We recognize that, listen, you had a full-service hospital in your community for over 100 years and suddenly it's gone. We certainly understand why people are frustrated by that," said Lynam. "But the reality is that there are no other providers stepping forward. We've put forward what we think is a realistic plan that will fill that void."
For the thousands of former St. Vincent's patients – particularly those without a lot of resources -- this offers little comfort. "I think it's a health crisis like a silent time bomb," said Kaufman. "It's just sitting there, brewing. It’s happening every day but it's hidden from the public eyes. … And I think it’ll get worse."
Whatever the Science Shows, Banning Smoking in Parks Makes Sense
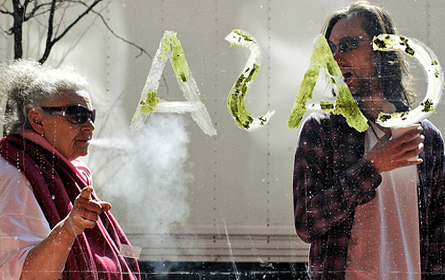
Smoking in New York City parks, beaches, and pedestrian malls became illegal last week. At a public hearing when the ban was proposed last fall, the city's health commissioner, Thomas Farley, predicted, "In the future we will look back on this time and say, 'How could we have ever tolerated smoking in a park?'"
Farley is almost certainly right. Public attitudes toward smoking have changed so thoroughly in the last 40 years that the smoke-filled offices depicted in "Mad Men" are barely recognizable. It’s likely that a few decades from now, if not sooner, the idea of smoking in a park will seem as outlandish as lighting up in an elevator or a supermarket -- the first public spaces in New York City where smoking was prohibited, 37 years ago.
Extending the Limits
It was in the spring of 1974 that New York City's health commissioner tried to ban smoking in "places of public gathering," such as restaurants, theaters, museums, libraries and hospitals. It was a radical proposal. Almost 40 percent of U.S. adults smoked, around double the rate today.
The resistance to the proposal was so intense that the law was dramatically weakened on the way to passage; the ban was whittled down to cover only elevators and supermarkets "There will be no more ashes flicked on raw meat in the meat departments," the commissioner, Lowell Bellin, said.
Over the following decades, however, public tolerance for smoking eroded, and most public spaces became smoke-free. Opinion polls have shown overwhelming support for the increasing limitations, even among smokers themselves.
Taking It Outside
Extending bans from enclosed spaces to outdoor areas represents a new phase. Yet a common thread connects the first restrictions on indoor spaces passed in the 1970s to the new laws on parks and beaches that have become increasingly common across the country: All these bans have dual rationales, but only one is usually acknowledged.
The first and most prominent rationale is to protect non-smoking bystanders from secondhand smoke. At first, this reasons was based more on suspicion than fact -- the scientific evidence of the dangers of secondhand smoke was scant in the early years of tobacco control -- but eventually studies demonstrated that exposure to the smoke of others was associated with elevated risk of cancer, heart disease and other illnesses.
The second purpose behind smoking bans, then and now, is less often acknowledged but almost equally important from the standpoint of public health: changing public attitudes. To reduce the toll of illness and death from cigarettes, tobacco foes sought to transform smoking from a glamorous, desirable behavior to a stigmatized, unacceptable one. In political debates over bans, this rationale was often soft-pedaled, although a few public health officials were blunt about their goal. Said Bellin when he was New York's health commissioner in 1974, "We hope to create a climate in which the smoker is uneasy."
The Power of Stigma
Bans on smoking in indoor spaces are unquestionably justified on health grounds. Outdoors, however, air-monitoring studies have shown that cigarette smoke dissipates and poses little risk to anyone more than a few feet away.
So it's clear that, whatever health claims proponents may make, the intent of banning smoking in parks is a social one: to "de-normalize" smoking. Testifying last fall on New York's law, health commissioner Farley made this clear when he said, "Parents should be able to bring their children to parks and beaches knowing that they won't see others smoking."
Some critics see this use of the law as unjustified, even sinister. But it's important to remember that the social climate decades ago when smoking seemed natural didn’t come about naturally -- it, too, was engineered. Throughout the 20th century, tobacco companies with vast resources at their disposal used aggressive marketing and advertising to portray smoking as a symbol of glamour and sophistication.
Public health advocates seeking to halt the epidemic of tobacco-related illness don't have anywhere near the financial clout that the tobacco industry does, but they can shape public opinion through laws and regulations. Banning smoking in public places such as parks and beaches sends a powerful symbolic message that smoking is unacceptable, even in situations where it poses no direct health risks to others.
James Colgrove is associate professor in the Center for the History and Ethics of Public Health at Columbia University's Mailman School of Public Health and author of Epidemic City: The Politics of Public Health in New York (Russell Sage Foundation, May 2011).




