Bed-Stuy Nursing Home: 'Much Below Average' in Staff Care

The Gotham Gazette examined inspection reports, complaints and court records to take a close look at five of the city’s lowest-rated nursing homes. This is the last of five parts.
When Harold Beer entered Bishop Henry Hucles Nursing Home, he gave his prosthetic leg to an aide while being fitted for a wheelchair. He says they never returned it.
“They also won’t tell me when they’re letting me go,” complained the 73-year-old Beer. “I can’t get a straight answer around here.”
Complaints about Bishop Henry Hucles are not uncommon. The facility, located in the Bedford-Stuyvesant neighborhood of Brooklyn, ranks as one of the lowest-rated nursing homes in the city, according to state inspections and Medicare records.
Bob DeVito, administrator of the 240-bed nursing home, rejects the findings of state inspectors who assigned the facility several poor scores in categories used to measure its performance.
“Those scores must be either outdated or wrong,” he said. “This nursing home takes great care of its residents.”
 The Centers for Medicare & Medicaid Services (CMS), which evaluates nursing homes, gave Bishop Henry Hucles an overall rating of two stars, which the CMS assigns to nursing homes that provide a “below average” level of care.
The Centers for Medicare & Medicaid Services (CMS), which evaluates nursing homes, gave Bishop Henry Hucles an overall rating of two stars, which the CMS assigns to nursing homes that provide a “below average” level of care.
DeVito would not allow a Gotham Gazette reporter to tour the facility, citing instructions from new owner, Michael Melnicke, whose company operates several nursing homes. Meinicke didn’t respond to requests for an interview.
The CMS gave Bishop Henry Hucles a one-star rating in the all-important staffing category. The CMS equates a one-star rating with a “much below average” level of care. The rating is based largely on the amount of time nurses and certified nurse aides spend each day with residents.
Arthur Edey, a former employee, claims that staffing problems began in 2011 when Episcopal Health Services, the non-profit that operated the nursing home, transferred ownership of Bishop Henry Hucles to Melnicke. The nursing home reduced staff to three certified nurse aides (CNA) for every floor, which have as many as 40 residents, he said.
“That’s a lot of people to cover, and some of them need lots of help,” Edey said. “It also means people have to wait longer to get the help they need.”
Staff also was asked to clean two floors per person, which “is an impossible thing to ask one person to do,” he added.
Bishop Henry Hucles admits many residents who need long term care and suffer from Alzheimer’s disease and dementia. A nurse who asked that her name be withheld because she feared that she could lose her job for commenting, said that when staff gets squeezed, “the care of the patients sometimes suffers.”
A typical nursing home needs an average of 4.4 hours of direct care staff time per resident per day to see positive outcomes, said Richard Mollot, a consumer advocate for nursing homes.
“If you dig into how CMS computes data, 4.4 hours translates to a high four- or a five-star rating,” Mollot said. “Three stars is significantly below average, and one star means you’re one of the worst in the country.”
At Bishop Henry Hucles, registered nurses spend an average of 18 minutes per day per resident, less than half the state average of 42 minutes and national average of 48 minutes. The facility’s licensed nurses spent an average of 59 minutes a day per resident, nearly 35 minutes less than the state average.
Unlike other states, New York does not have a mandated minimum staff ratio or a minimum amount of hours that nursing staff is required to devote to nursing home residents (although there is a proposed bill that aims to change that), Mollot said.
Staffing deficiencies can lead to patient neglect. For example, a resident walked out of Bishop Henry Hucles undetected on Dec. 18, 2012, according to a state inspection report. The resident typically strolled inside the facility at about 7:30 p.m. and nursing aides assumed she was on the first floor, the report says. It is unclear how long it took the home to locate the resident, but she wasn’t reported missing until 11:20 p.m., according to the report.
The facility scored low in several care categories. There has been a 41-percent increase in the number of long-term residents who need help with daily activities, according to CMS data. The statewide average is 15 percent. Nearly 36 percent of the residents exhibit symptoms of depression – three times the state average of 11.7 percent, the CMS data show.
Health violations have also been a problem at the home. Inspectors cited Bishop Henry Hucles for 12 health deficiencies last year, more than double the 5.3 state average. For example, a licensed practice nurse (LPN) left medications unattended in a hallway while she went to the medication room. The LPN left the cart unattended again 10 minutes later. In another case, a resident with a skin rash was ordered to see a dermatologist, but didn’t see one until 16 weeks later because of multiple miscommunications among staff.
On a recent visit to Bishop Henry Hucles, residents were dressed in tattered clothing. A few residents said the home’s food was extremely poor and wished there was more variety.
“All they ever give us is gravy, gravy, gravy,” said Sally Norman, a longtime resident. “It’s not good for us.”
Some staff members at the home are also unhappy. Edey, a 15-year employee at Bishop Henry Hucles, complained that Melnicke instituted a few unwelcome changes when he took ownership of the facility.
“They had added changes to our union contracts,” he said. “And they weren’t good.”
The changes included fewer overtime hours and lower disability benefits, Edey said. Melnicke was unwilling to compromise on the changes, said Edey, who was the union representative.
“We voted the changes down,” Edey said. “But Melnicke said no one had ever voted against him, and we had to vote over.”
The next vote was an even more resounding no.
Edey, 61, had spent six months on disability after spraining an ankle and tearing an ACL on the job. He said that after the union vote Melnicke went to his supervisor and said he didn’t think Edey was healthy enough to continue working, even though Edey’s doctor had advised him to go back to work.
“I’ve been on disability ever since,” he said.
Alex Eidman filed this report while attending the CUNY Graduate School of Journalism.
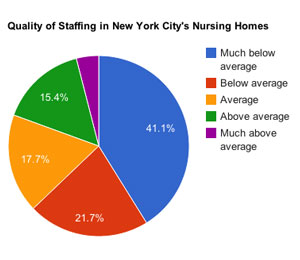
The "Quality of Staffing" pie chart uses data obtained from the Centers for Medicare and Medicaid Services.
'Tax Dollars are Paying for This'

The Gotham Gazette examined inspection reports, complaints and court records to take a close look at five of the city’s lowest-rated nursing homes. This is the third of five parts.
Citing a pattern of serious problems, federal regulators placed Marcus Garvey Nursing Home on an exclusive watch list of the worst nursing homes in the country in 2009 and again in 2011.
Those actions occurred while the state attorney general’s office pursued a civil lawsuit accusing Ruby Weston, the facility’s owner, of using money intended for resident care to enrich herself and her family. A 2012 settlement of the lawsuit required Weston to forfeit $821,000 in deferred compensation and pay $50,000 to cover the cost of the AG’s investigation.
The 295-bed nursing home in Brooklyn’s Crown Heights neighborhood is now named the Marcus Garvey Residential Rehab Pavilion and operated by new owners. Yet it remains one of the worst in the country.
Current administrators say they are working to solve the problems but seem to have a lot to overcome.
In 2009, the federal oversight agency for Medicaid and Medicare designated Marcus Garvey a Special Focus Facility (SFF) after an investigation found that its staff was failing to properly administer patients’ medications. The nursing home was fined nearly $55,000.
The facility landed on the SFF list the following year after regulators found that Marcus Garvey staff failed to report a resident’s high potassium levels, body numbness, and trouble breathing. The resident was hospitalized and died. Soon after that, the state fined the facility $20,000 for delivering sub-standard care.
When Marcus Garvey was placed on the SFF watch list, its administrators were told they need to make significant improvements to continue to receive Medicare funds. They needed to hire more competent staff, for example, and make clear policies to ensure patients receive the proper medications, according to Medicare documents. But the problems persisted.
“People are suffering and our tax dollars are paying for this,” said Richard Mollot, leader of the advocacy group Long Term Care Community Coalition.
Substandard nursing homes such as Marcus Garvey are supposed to lose their Medicare and Medicaid money if they fail to correct serious problems, Mollot said. Government agencies are failing to enforce their regulations, he said.
Quality of care measures
Despite the fines and additional oversight, Marcus Garvey remains among the lowest ranking nursing homes in the city. One of the most troubling problems fueling its poor ratings is the large number of patients on antipsychotic drugs.
Aproximately 40 percent of the long-term patients at Marcus Garvey receive antipsychotics — more than twice the state average, according to state Health Department records. And 4.6 percent of the facility’s short-term patients take the drugs, well above the 2.7 percent state average.
Elder care advocates and doctors have said antipsychotic drugs, which include powerful tranquilizers such as Risperdal and Seroquel, are often overused in nursing homes as chemical restraints.
Marcus Garvey Medical Director Pierre Brutus said he is trying to reduce the number of patients on antipsychotics. However, doing so is difficult because the nursing home receives many patients from Gracie Square Hospital, a psychiatric and substance abuse facility in Manhattan, he said.
Hospital adminstration said it could not provide information about the number of patients transferred to Marcus Garvey.
Two-thirds of Marcus Garvey’s long-term residents display symptoms of severe depression, federal records show. That’s nearly six times higher than the state average and 11 times higher than the national average. Brutus said that for many of these patients, there is nothing the facility can do.
“Some have major depression, and we cannot reverse that,” he said.
Federal inspectors routinely found problems at Marcus Garvey that could be reversed. A Gotham Gazette review of federal inspection reportds from 2011 to 2012 found many other violations, including the failure to:
- Properly administer medications (one insulin-dependent resident’s chart showed no evidence that she had received insulin for three days in a row);
- Provide proper dental services (during the state inspection, a resident told an inspector that she was missing her front teeth because of a fall and hadn’t seen a dentist during her year-long stay at the facility);
- Address “critical and aberrant” lab results;
- Do an accurate assessment of each patient and keep each resident — along with his or her doctor and family — apprised of any changes in health status (one resident’s health care manager told inspectors that the facility “does not always inform him about changes in the resident's medication or treatment”).
Yoga instructor Daniela Bella discovered how frustrating it could be to try to improve conditions at Marcus Garvey. Once a week, she guided a classroom of residents in “chair yoga,” in which the elderly participants go through a series of stretches and poses while seated in chairs.
“They were happy, they loved the music and they loved me,” Bella recalled. “I got close with a lot of them,” she said.
Despite the patients’ enthusiasm, Marcus Garvey administrators often forgot to tell residents about scheduled classes or failed to clear the classroom of furniture, she said. It simply wasn’t a priority, she said.
“You could tell they had just forgotten,” Bella said.
The Marcus Garvey website prominently features a photo of the facility’s visitor lounge. “Visitors welcomed and encouraged everyday,” reads the photo caption. But a visit by the Gotham Gazette was clearly unwelcome; its reporter was escorted out of the building.
An apologetic Gloria Gasper, director of social work at the home, said a few days later that interviews with residents and staff are not allowed.
“I just think this is a place that has its own culture,” she said. “I would suggest you not waste your time here.”
Erin Brodwin filed this report while attending the CUNY Graduate School of Journalism.
Manhattan Nursing Home Rates Low in Health Care

The Gotham Gazette examined inspection reports, complaints and court records to take a close look at five of the city’s lowest-rated nursing homes. This is the second of five parts.
When Wayne Padgett’s aunt ended up at the Mary Manning Walsh Nursing Home on the Upper East Side last spring, he never imagined that he would eventually need to fly across the country to rescue her.
His 86-year-old aunt, Geraldine McCandless, had been sent to recover at the nursing after being hospitalized for a stroke. Padgett was not happy with what he saw when he flew from his California home to visit her.
“When I arrived in New York, I was horrified,” he said. “The place is dirty and run down. The staff do not really care and they have attitudes against asking for help.”
To document his point about the cleanliness issue, Padgett photographed the stained carpets and walls at the facility. He also said that he saw residents left in their wheelchairs in the hall all day, lined up in front of the nursing station with nothing to do.
“They were left in the hall to rot,” he said.
Mary Manning Walsh is one of the lowest-rated nursing homes in Manhattan, according to the federal Centers for Medicare & Medicaid Services (CMS). It is one of the two nursing homes in Manhattan rated one star (out of five) in the health inspection category. The CMS equates one star with "much below average" care. The average health inspection rating for the 18 nursing homes in Manhattan is 3.5 stars.
The CMS gave the facility only two stars (out of five) for overall quality, whereas the average rating in the borough is four stars. The CMS equates two stars with below average care.
A higher-than-average percentage of short-term residents at the 362-bed nursing home suffer problems with bedsores, according to data compiled by the New York State Department of Health. The data show that 2.2 percent of residents at the facility have bedsores that are "new or worsened," compared to an average of 1.4 percent statewide and 1.3 percent the nationwide.
Leonard Rosner, a former patient at Mary Manning Walsh, is suing the nursing home for what he says was a failure to prevent and treat his bedsores. Nurses neglected to treat him even when his bedsores began to emit an odor.
“All you need to do is use your nose,” said Rosner’s attorney Jonathan Fairbanks, suggesting that his client’s condition was easy to detect. “In Rosner’s case, they waited three weeks before making a referral.”
In another health-related matter, Mary Manning Walsh was fined $6,500 last year for excessively hot water in the sinks in residents’ rooms. State inspectors measured water temperatures as high as 136 degrees – hot enough to blister the skin after 10 seconds of exposure, according to safety guidelines.
The hot water hazard was first reported to the administration in April 2012, but it still had not been fixed when the inspectors came to the nursing home the following year.
Other deficiencies reported by CMS and state Health Department in the past three years include errors in administering medication, failure to report medication errors and failure to store and cook food in a safe way. Inspectors also reported that 15 percent of the residents at Mary Manning Walsh exhibit symptoms of depression, compared to an average of 12 percent statewide and 6.6 percent nationwide.
Jon Goldberg, the spokesperson for ArchCare, the health care ministry for the Archdiocese of New York, suggested that the facility’s low rating by CMS is not indicative of the care it has provided in the past.
“Historically, the Mary Manning Walsh Nursing Home has had five-star ratings,” he said.
Administrators and the owners of the facility didn’t respond to several requests for an interview.
The problems at Mary Manning Walsh are indicative of the substandard quality of care prevalent in nursing homes across the state. New York ranked 45th out of all states this year in Home Report Cards, a ranking compiled by Families for Better Care, a Florida-based advocacy group.
“The blame really starts with individual owners first,” said Brian Lee, the organization’s executive director.
But he added that the lack of appropriate legislation with regard to staffing levels on a state level exacerbates the problem. Unlike some states, New York has no specific staffing requirement and instead allows nursing homes leeway in deciding how many staff members they employ.
“Far too many people are left in danger,” Lee said.
In Wayne Padgett’s opinion, leaving his aunt in Mary Manning Walsh posed a danger to her health. He decided to move her into a home in California. That proved unnecessarily difficult because administrators at Mary Manning Walsh couldn’t locate such important documents as power of attorney, he said.
When his aunt was finally transferred, her new home discovered that a deep cough she had developed was a symptom of bronchitis which the staff at Mary Manning Walsh had failed to diagnose, Padgett said.
His aunt is doing better at her new nursing home, Padgett reports.
“People here are sweet and they care,” he said about the staff.
___
Agata Blaszczak-Boxe is a freelance journalist and graduate of CUNY Graduate School of Journalism.




